
Experiencing upper leg pain is a common concern. You might wonder about its severity. This blog aims to demystify your upper thigh pain. We will outline its causes, effective relief strategies, and crucial indicators for seeking professional medical attention.
Your symptoms are key for proactive health management. While many cases of thigh pain are mild, stemming from simple muscle strains, others can be more serious, involving nerve issues like sciatica or even a dangerous blood clot. Understanding these differences helps you know when to act for your health.
Key Takeaways
Recognize urgent signs like sudden, severe pain, numbness, or swelling. These mean you need to see a doctor right away.
Understand common causes of upper leg pain. These include muscle strains, nerve issues like sciatica, and arthritis.
Use home remedies for mild pain. Try the RICE method, gentle stretches, and over-the-counter pain relief.
Seek professional help if pain lasts too long or gets worse. Also see a doctor if pain stops you from daily activities.
Urgent Signs of Upper Thigh Pain
You need to recognize certain symptoms of upper thigh pain. These signs tell you to seek immediate medical help. Ignoring these signals can lead to serious health problems. Pay close attention to your body.
Sudden, Severe Pain
Sudden, very bad pain in your upper thigh demands attention. This type of pain often comes on quickly. It might feel like a sharp, intense ache. If this severe pain does not get better within a few days, you should see a doctor. This could be a sign of a serious condition, like a blood clot. A blood clot in your leg can be very dangerous.
Numbness or Weakness
You might feel numbness or weakness in your thigh. This means you cannot feel your leg well, or you have trouble moving it. Persistent numbness or weakness is not normal. Several neurological conditions can cause these feelings.
Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, often starts with muscle twitching and leg weakness.
Toxic neuropathy can damage nerves in your legs. Toxins like cleaning chemicals, insecticides, heavy metals, or too much alcohol cause this. You might feel numbness, tingling, and weakness.
Myasthenia gravis (MG) is a disorder that causes muscle weakness. It can affect your arms, hands, legs, or feet.
Swelling and Discoloration
Look for swelling in your upper thigh. Your leg might look larger than usual. You might also see discoloration, like redness or bruising. These symptoms can point to a serious issue. A blood clot can cause swelling and changes in skin color. You need to get this checked right away.
Fever or Chills
If you have upper thigh pain along with a fever or chills, you might have an infection. Your body uses fever to fight off germs. Chills often come with a fever. An infection in your leg can be serious. You need medical care to treat it.
Inability to Bear Weight
You might find you cannot put weight on your leg. This means you cannot stand or walk without severe pain. This symptom often points to a significant injury.
Ligament tears in your knee can make it hard to bear weight.
Fractures, or broken bones, in your knee or tibia commonly prevent you from putting weight on your leg.
Meniscus injuries, which are tears in your knee cartilage, also cause this problem.
A patellar dislocation happens when your kneecap moves out of place. This makes bearing weight very difficult.
Accompanying Systemic Symptoms
Sometimes, upper thigh pain comes with other body-wide symptoms. These are very serious. Seek immediate medical help if you experience:
Anxiety
Clammy skin
Chest pain
Fainting
An irregular heartbeat
Lightheadedness
A weak pulse
These symptoms can signal a medical emergency. They might mean problems with your heart or circulation.
Loss of Bowel or Bladder Control
This is a critical sign. If you lose control of your bladder or bowels along with upper leg pain, you need emergency care. This can be a symptom of Cauda Equina Syndrome (CES). CES is a medical emergency. It happens when nerves at the end of your spinal cord get compressed.
Symptoms of CES include lower back pain and/or leg pain (sciatica). You might also have leg weakness.
You can feel numbness or strange sensations like burning, prickling, or tingling. These feelings often occur in the backs of your legs, butt, hip, and inner thighs. This is called paresthesia.
Urinary and/or fecal incontinence or retention are key signs. You might not control your urine or stool, or you might have trouble passing them.
Immediate medical attention is crucial for CES. Doctors often need to perform surgery quickly. This helps prevent permanent damage. Without fast treatment, you could face paralysis or ongoing loss of bowel or bladder control.
Common Causes of Upper Leg Pain

Many different issues can cause upper leg pain. Understanding these causes helps you know what might be happening in your body. Sometimes, simple things like flat feet, rigid arches, or even the wrong footwear can contribute to leg pain.
Muscle Strains and Sprains
You might experience a muscle strain or sprain in your upper leg. This happens when you overstretch or tear muscle fibers or ligaments. You often feel sudden pain, tenderness, and sometimes bruising.
Most muscle injuries will feel less sore and more functional within 6-10 weeks, though the healing process can continue for several months beyond that. Mild or moderate strains in your legs may take up to 8 to 10 weeks or more to heal. If you have a severe (Grade III) strain, symptoms might last until the torn muscle heals or you have surgery.
Grade I muscle strain: You typically recover within 2 to 4 weeks.
Grade II muscle strain (partial tear): This may take 6 to 8 weeks to heal.
Grade III muscle strain (complete tear): You may need up to a year for full recovery. This type might also require surgery.
Sciatica and Nerve Issues
Sciatica is a common cause of pain in your thigh. It happens when your sciatic nerve gets irritated. This nerve is the longest and thickest in your body. It runs from your lower back, through your hip and buttock, and down your leg.
Sciatica pain can occur anywhere along this nerve’s path, even extending to your feet and toes. Sciatica that goes down your legs, often past your knee, usually means you have a pinched nerve in your back.
Arthritis in your back can cause degenerative changes. These changes can narrow the space inside your backbone, a condition called stenosis. This irritates the nerve roots going to your legs.
A herniated disc is another frequent cause. A small or large disc herniation can pinch a nerve in your back. Your brain then interprets this as leg pain. Sciatica often results from irritation of spinal nerve roots.
Doctors also call this nerve compression, a pinched nerve, or entrapment neuropathy. When the irritated nerve roots are in your lower back, it is called lumbar radiculopathy. Disc tissue or bone spurs often compress the nerve. Other things can also compress nerves. These include fractured bone fragments, tumors, infections, or inflammation. Common causes of spinal nerve root compression include:
A herniated disc (ruptured or slipped disc). Here, the gel-like center of an intervertebral disc pushes through a tear. This puts pressure on the nerve root(s) nearby.
Spinal stenosis. This is a narrowing of the canal that holds your spinal nerves.
Less commonly, the sciatic nerve itself gets compressed outside your spine. This can happen due to bone or muscle injuries, like a fractured hip. Diseases like tumors or infections, pregnancy, orthopedic hip surgery, or piriformis syndrome can also cause this.
Tendinitis and Bursitis
Tendinitis and bursitis can cause pain in your thigh. Tendinitis is inflammation of a tendon. Bursitis is inflammation of a bursa. A bursa is a small, fluid-filled sac that cushions bones, tendons, and muscles near your joints.
Trochanteric bursitis occurs when a bursa near your hip joint becomes irritated. Specifically, it affects the bursa covering the greater trochanter. This is the pointed upper, outside edge of your thigh bone (femur) where it connects to your pelvis. The trochanteric bursa is one of the largest in your body.
It is on the prominent bone (greater trochanter) on the upper outside portion of your thigh. This bursa experiences significant stress and friction from surrounding muscles and tendons. Trochanteric bursitis affects the outside part of your hip.
Arthritis and Joint Problems
Arthritis can cause significant upper leg pain. It affects your joints, leading to inflammation and discomfort.
Osteoarthritis (OA): This involves the gradual wearing away of cartilage in your joints. It commonly affects your knees, hips, and lower back, leading to leg pain. This type results from the natural aging process. It wears away cartilage in your joints. It commonly affects both your hips and knees, causing inflammation and pain.
Rheumatoid arthritis (RA): This is an autoimmune disease. Your immune system attacks healthy cells, causing inflammation. It frequently affects your hips, knees, ankles, or feet. This can result in leg pain. This immune system problem attacks cartilage in your joints. It typically affects both sides of your body, impacting both your hips and knees.
Infectious (septic) arthritis: This happens when an infection from another part of your body travels to a joint. It most often affects your knees, thus impacting your legs.
Polymyalgia rheumatica: This is an arthritis-related condition. It involves inflammation of bursae around your joints. It can cause pain and stiffness in your hips, pelvis, thighs, and sometimes your knees.
Post-traumatic arthritis: This is a form of osteoarthritis. It develops after an injury to your hip or knee, possibly years later.
Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis (DVT) is a serious condition. It involves a blood clot forming in a deep vein, usually in your leg. This blood clot can cause pain, swelling, and warmth in your thigh. If you suspect a blood clot, seek immediate medical attention. A DVT can be life-threatening if the blood clot travels to your lungs.
Peripheral Artery Disease (PAD)
Peripheral Arterial Disease (PAD) affects blood flow to your limbs. It happens when narrowed arteries reduce blood flow to your arms or legs. This causes pain, especially during exercise. A key indicator for PAD is pain that consistently occurs during exercise and subsides shortly after you stop.
The ankle-brachial index (ABI) of 0.90 or less is used as a diagnostic tool for Peripheral Artery Disease (PAD).
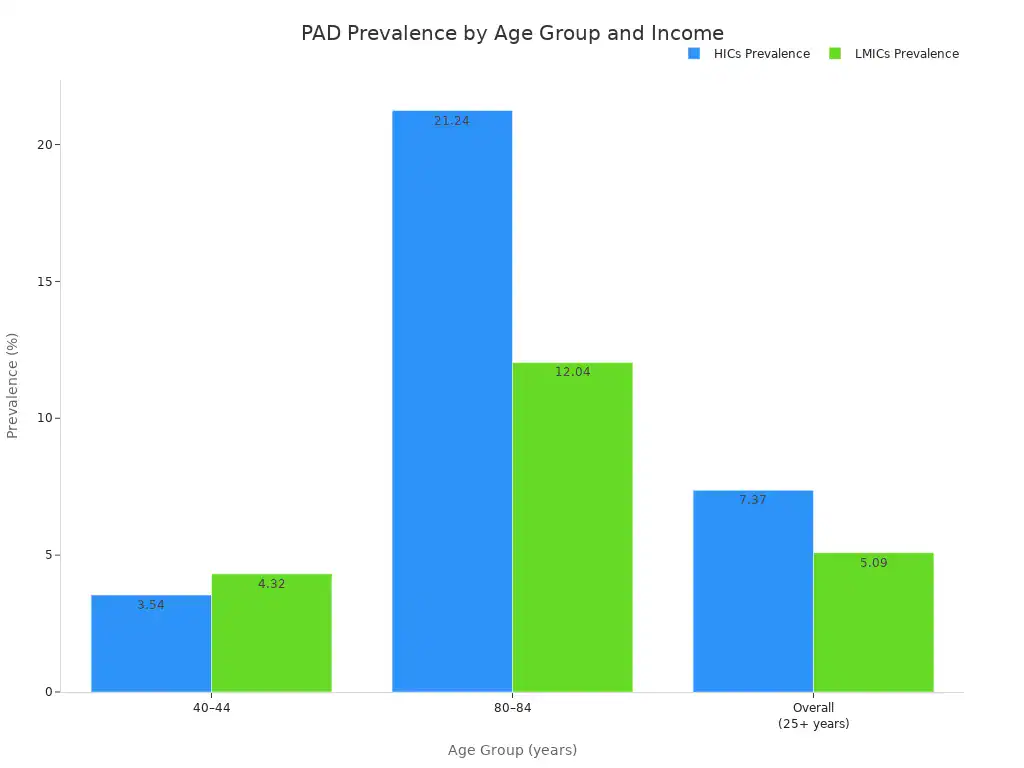
Here is a look at the prevalence of PAD across different age groups and regions:
Age Group (years) | HICs Prevalence (%) | LMICs Prevalence (%) | Global Prevalence (%) | Males (per 100,000) | Females (per 100,000) |
|---|---|---|---|---|---|
40–44 | 3.54 | 4.32 | N/A | 332.32 | 621.11 |
55–59 | N/A | N/A | 6.40 (men) / 6.37 (women) | N/A | N/A |
80–84 | 21.24 | 12.04 | N/A | N/A | N/A |
95+ | N/A | N/A | N/A | 17,195.57 | 24,965.3 |
Overall (25+ years) | 7.37 | 5.09 | 5.56 | N/A | N/A |
In 2010, the estimated global prevalence of PAD was around 202 million worldwide. Approximately 70% of the affected population lived in low-income and middle-income countries (LMICs). In 2015, the estimated total number of people aged 25 years and older suffering from PAD was 236.62 million worldwide. 72.91% lived in LMICs. Women were slightly more affected globally. They accounted for 52.23% of the PAD population in 2015. The prevalence of PAD generally shows a marked increase with age, especially above 65 years.
Stress Fractures
Stress fractures are tiny cracks in a bone. They often result from repetitive force, like running or jumping. You might feel a dull ache that worsens with activity. These fractures are common in the bones of your leg.
Cramps and Electrolyte Imbalances
Muscle cramps are sudden, painful contractions of your muscle. They often occur in your thigh. Electrolyte imbalances can cause these cramps. Electrolytes are minerals like sodium, potassium, magnesium, calcium, and chloride. They help your body function properly.
Decreases in the concentration of sodium, potassium, magnesium, chloride, and/or calcium are suggested as causative factors for exercise-associated muscle cramps (EAMCs).
Carbohydrate-electrolyte beverages containing sodium, potassium, and chloride can delay the onset of EAMCs.
Diabetic Neuropathy
Diabetic neuropathy is a type of nerve damage. High blood sugar levels cause it. This condition often affects the nerves in your legs and feet. You might experience pain, tingling, numbness, or weakness in your thigh. This pain can be constant or come and go. Diabetic neuropathy is a serious complication of diabetes.
Acute Trauma and Joint Injuries
Acute trauma can cause significant upper leg pain. This refers to sudden, severe injuries. These injuries can affect your bones, muscles, ligaments, or joints. A thigh condition resulting from trauma can be very painful.
Blunt trauma accounts for 73% of cases.
Penetrating trauma and gunshot wounds make up 11% of cases.
Motor vehicle collisions are involved in 48% of patients.
Ipsilateral femur fractures occur in 42% of blunt trauma cases.
Other causes include crush injury, thigh contusion, and vascular injury. Trauma is the most common cause. Ipsilateral femur fractures, especially open fractures, have an increased incidence. Crush injuries, contusions, and gunshot wounds are also common. Any significant trauma to your leg can lead to problems felt in your thigh.
Effective Relief for Thigh Discomfort
You can find effective relief for your thigh discomfort with several self-help measures. Many new thigh problems often resolve within six weeks without professional medical intervention.
RICE Method Application
The RICE method (Rest, Ice, Compression, Elevation) helps manage acute injuries. For ice application, use a cold pack. Apply it for 15-20 minutes every 2-3 hours during the first 24-48 hours after your injury. This reduces swelling and helps with pain. You can also apply ice for 10 minutes, stop for 20 minutes, and then reapply in this cycle one or two more times. Remember to use a skin barrier with the ice pack.
Gentle Movement and Stretching
Gentle movement can ease discomfort, especially from pins and needles. Stretching also helps with muscle cramps. Try these stretches for your thigh:
Hamstring Stretch: Sit on the ground with straight legs. Bend at your waist, keeping your chest open and back long. Slide your hands towards your feet. Hold for 30 seconds.
Quadriceps Stretch: Hold onto a wall for balance. Stand on one leg. Lift the opposite leg, gently bend the knee, and pull your foot close to your buttock. Hold for 30 seconds. Repeat with your other leg.
Inner and Outer Thigh Stretch: Stand with feet shoulder-width apart. Lunge to the left, bending your knee to 90 degrees. Keep your knee from going past your toes. Lower into the side and straighten your right leg. Place your hands on your left thigh and hold for 30 seconds. Straighten up and repeat on the opposite side.
Over-the-Counter Pain Relief
Over-the-counter (OTC) medications can help manage pain. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen reduce both pain and inflammation. Acetaminophen can also relieve pain. Always follow the dosage instructions on the label.
Heat and Cold Therapy
Alternating heat and cold therapy can provide relief. Cold therapy reduces inflammation, while heat therapy relaxes muscles and improves blood flow. You can apply each for about 15-20 minutes. There are no strict rules for timing. Adjust based on your personal preference and how your body responds. This combination can help reduce pain and increase blood flow in your muscles.
Massage and Foam Rolling
Massage and foam rolling can target tight muscles in your thigh.
Quads: Use a foam roller to alleviate tightness in your quadriceps.
Hip Flexors: Lie face down. Place the foam roller under your hip flexor. Roll slowly up and down and side to side for 30 seconds. Focus on tender spots.
Hamstrings: Sit with legs extended. Place the foam roller under your hamstrings. Lift your body and roll up and down between the back of your knees and glutes for at least 30 seconds. Linger on tender spots.
Lifestyle Adjustments
Making lifestyle adjustments can prevent and reduce thigh problems. Wearing appropriate footwear is crucial. Shoes that are too tight, too loose, or lack support can disrupt your natural body alignment. This can lead to chronic pain in your legs. Address foot structure issues like flat feet or rigid arches with supportive footwear.
Hydration and Nutrition
Proper hydration and nutrition are essential home remedies for muscle health. Dehydration can contribute to muscle cramps. Drink plenty of water throughout the day. Certain nutrient deficiencies can also cause leg pain.
Calcium and Vitamin D: These are vital for strong bones and muscle function. Deficiencies can cause muscle aches and weakness.
Magnesium and Potassium: These electrolytes are crucial for preventing muscle cramps and spasms.
B Vitamins and Iron: Deficiencies in these can lead to nerve pain, tingling, or muscle fatigue.
Medical Interventions and Diagnostics

When self-care does not help your upper leg pain, doctors have many tools. These medical interventions help diagnose and treat your discomfort. They aim to find the cause of your pain and offer effective solutions.
Physical Therapy Referrals
Your doctor might send you to physical therapy. A physical therapist helps you with exercises. These exercises strengthen your muscles and improve flexibility. They can teach you how to move better. This helps reduce your pain and prevent future problems. Physical therapy is a common treatment for many types of leg pain. It supports your long-term recovery.
Prescription Medications
For chronic upper leg pain, especially nerve pain, doctors may prescribe specific medications. These are often drugs first made for other conditions.
Anticonvulsants: These include carbamazepine (Tegretol), gabapentin (Neurontin), lamotrigine (Lamictal), and pregabalin (Lyrica). They help block pain signals in your nerves.
Antidepressants:
Tricyclics: Such as amitriptyline (Elavil), doxepin (Sinequan), and nortriptyline (Pamelor).
SNRIs (Serotonin–norepinephrine reuptake inhibitors): Like duloxetine (Cymbalta), milnacipran (Savella), and venlafaxine (Effexor).
SSRIs (Selective serotonin reuptake inhibitors): Fluoxetine (Prozac) is one example, though its pain relief evidence is mixed. These medications can significantly help manage your pain. Doctors start with low doses and slowly increase them. It can take weeks to see their full effect. These pain treatments can be taken daily.
Injections and Procedures
Sometimes, injections can help with localized pain. Your doctor might suggest steroid injections. These reduce inflammation in a specific area. Nerve blocks can also stop pain signals. These procedures offer targeted relief for your pain.
Advanced Imaging (X-ray, MRI)
Doctors use imaging tests to see inside your body.
X-rays show bones. They can find fractures or arthritis.
MRI (Magnetic Resonance Imaging) gives detailed pictures of soft tissues. MRI is the best way to see muscle injuries in your hip and thigh. It shows swelling, blood clots, or tears. Advanced MRI techniques can also look at nerve problems. They help find nerve entrapment syndromes in your leg. High-resolution ultrasonography (US) also helps doctors see nerves and surrounding structures clearly.
Nerve Conduction Studies
If your doctor suspects nerve damage, you might have a nerve conduction study. This test measures how fast electrical signals travel through your nerves. It helps find nerve damage or compression. This test can pinpoint the cause of your nerve-related pain.
Blood Tests and Lab Work
Blood tests can reveal underlying conditions. They can check for inflammation, infection, or specific diseases. For example, blood tests can help diagnose certain types of arthritis or electrolyte imbalances. These tests give your doctor more clues about your pain. They guide your treatment plan.
When to Seek Professional Help for Upper Leg Pain
You need to know when to see a doctor for your upper leg pain. While many issues resolve on their own, some signs mean you need professional help. Do not ignore these signals.
Persistent or Worsening Pain
Your pain should not last forever. If your upper thigh pain continues for more than 72 hours, you should seek specialist medical advice. Pain that gets worse over time, instead of better, is also a red flag. This could signal a more serious condition. Pay attention if the pain occurs during or after walking.
Pain Affecting Daily Life
Pain should not stop you from living your life. If your upper leg pain makes daily activities hard, you need to see a doctor. This includes walking, working, or even sleeping. When pain limits your normal routine, it is time for professional evaluation.
Recognizing Symptoms of Upper Thigh Pain
You must recognize specific symptoms. If you notice swelling in both legs, this needs medical attention. Other urgent signs, like those mentioned earlier, also mean you should see a doctor right away. These include sudden, severe pain or numbness.
No Improvement with Self-Treatment
You might try home remedies for your thigh problems. However, if your symptoms do not improve after a few days of self-treatment, seek help. New or recurring thigh pain should typically start to improve within six weeks without needing professional medical intervention. If your pain persists beyond this, it is time to consult a healthcare provider.
Condition/Severity | Non-Surgical/Conservative Recovery Timeline |
|---|---|
Mild Cases | 2–4 weeks |
General Upper Leg Pain | 4–6 weeks |
Moderate to Severe Cases | 6–8 weeks |
Recurrent Thigh Problems
Do your thigh problems keep coming back? If you experience repeated episodes of upper thigh pain, you should talk to a doctor. Recurring pain often points to an underlying issue that needs proper diagnosis and treatment.
Upper leg pain has diverse causes, ranging from mild to serious. You must recognize your symptoms. Apply appropriate relief measures for your thigh. Most critically, know when to seek professional medical advice for your pain. Listen to your body. Consult healthcare providers for accurate diagnosis and personalized treatment plans. Early intervention prevents complications and improves outcomes for any upper leg pain. This helps manage your upper thigh pain effectively.




