
Experiencing a “brain burning feeling” can be unsettling and often alarming. This sensation might involve tingling, heat, pressure, or a pins-and-needles feeling in the head or scalp.
Studies show that 25% to 70% of people report head or scalp sensations like burning or tingling. This brain discomfort, while sometimes benign, always warrants attention. This blog explores potential causes, diagnostic approaches, and crucial indicators for seeking medical help regarding these symptoms.
Key Takeaways
A “brain burning feeling” is a nerve sensation, not actual heat. It means nerves send signals that the brain interprets as warmth or irritation.
Many things can cause this feeling. Stress, headaches, not drinking enough water, and tired feelings are common reasons. Scalp problems or medicine side effects can also cause it.
Sometimes, a brain burning feeling can be serious. Nerve damage, brain swelling, or diseases like multiple sclerosis can be the cause. These need a doctor’s attention.
See a doctor if the burning feeling starts suddenly or is very strong. Also, get help if you have other symptoms like weakness, vision changes, or trouble speaking. A doctor can find the cause and help you feel better.
Understanding the Brain Burning Feeling
Defining the Brain Burning Feeling
A “brain burning feeling” describes a specific type of neurological sensation. It is important to understand that this feeling is not actual heat. The brain itself does not have pain receptors in the same way skin does. Therefore, the sensation of burning does not mean the brain is literally on fire. Instead, it represents a subjective experience.
This experience arises from nerve signals. These signals misinterpret or overreact to stimuli. They create a perception of intense heat or irritation within the head or scalp. This sensation is a form of neurological discomfort.
How the Sensation Feels
People describe the brain burning feeling in many ways. Some individuals report a constant, low-level burning sensation. Others experience sharp, intense bursts. The feeling can manifest as a tingling sensation. It might also feel like pressure building inside the head.
Many describe it as a “brain on fire” feeling. This phrase captures the intensity and distress it causes. The burning can be localized to one area of the head. It can also spread across the entire scalp.
Sometimes, it feels like pins and needles. Other times, it is a deep, internal burning. This burning sensation can come and go. It can also persist for long periods. The exact nature of the burning feeling often provides clues about its underlying cause.
Common and Benign Causes
Many factors can cause a brain burning feeling. Often, these causes are not serious. They relate to everyday experiences or common health issues. Understanding these common causes can help ease worry.
Stress, Anxiety, and Hyperstimulation
Emotional states significantly impact physical sensations. High levels of stress and anxiety often trigger physical symptoms. A brain burning feeling can be one of these symptoms. When a person experiences stress, their body goes into a “fight or flight” mode. This response increases nerve sensitivity.
Nerves become more alert. This can lead to sensations like tingling, numbness, or burning.
Anxiety also causes blood vessels to expand. This process is called vasodilation. It improves blood flow. This increased blood flow can create a warm or burning sensation on the skin.
The body releases stress hormones like cortisol and adrenaline during anxiety. These hormones affect skin sensitivity. They contribute to inflammatory responses. These responses can manifest as a burning sensation. Psychological factors also play a role.
Heightened awareness of bodily sensations during anxiety can amplify normal feelings. Even mild discomfort or burning can feel more pronounced. Managing stress levels can often reduce these sensations.
Headaches and Migraines
Headaches and migraines are common causes of head sensations. Many people experience a burning feeling during or before these events. Tension headaches can cause a tight, burning sensation around the head.
Migraines, known for intense pain, can also involve burning or tingling. This happens because of nerve activation and changes in blood flow in the brain. The nerves become overactive.
This sends unusual signals. These signals are interpreted as burning. Some people describe a “hot” feeling in their head during a migraine attack. This pain can be quite intense.
Dehydration and Fatigue
The body needs enough water to function correctly. Dehydration can lead to various physical symptoms. A brain burning feeling can be one of them. When the body lacks sufficient water, the brain does not receive an adequate supply of oxygen. This deficiency in oxygen can result in pain.
This pain may be intermittent or constant with ongoing dehydration. Dehydration also significantly reduces blood volume. This impairs blood circulation. Essential nutrients cannot reach the brain effectively. This disrupts brain function. Reduced blood flow also compromises oxygen delivery to the brain.
Oxygen is vital for proper brain operation. A deficiency can cause numerous problems. Dehydration can also lower blood pressure and increase heart rate. All these factors contribute to unusual head sensations.
Fatigue also plays a role. When a person is extremely tired, their body and brain struggle to function optimally. This can lead to heightened sensitivity. It can also cause unusual sensations, including a burning feeling. Lack of sleep increases stress on the body. This stress can manifest as physical symptoms.
Scalp Irritation and Conditions
Sometimes, the burning feeling originates from the scalp itself. Various conditions can irritate the scalp. This irritation leads to burning or tingling sensations. Common scalp conditions that can cause burning or tingling sensations include:
Dermatitis
Psoriasis
Seborrheic dermatitis
Folliculitis
Head lice (Pediculosis capitis)
Ringworm (Tinea capitis)
Impetigo (bacterial skin infection)
Scabies
Alopecia areata
These conditions cause inflammation or nerve irritation on the scalp. This irritation sends signals to the brain. The brain interprets these signals as a burning sensation. Even harsh hair products or allergic reactions can cause temporary scalp irritation. This irritation leads to a burning feeling.
Medication Side Effects
Certain medications can cause a brain burning feeling as a side effect. These medications affect the nervous system. They can alter nerve signals. This leads to unusual sensations. Some common culprits include:
Certain antidepressants
Some blood pressure medications
Nerve pain medications
Chemotherapy drugs
Always review medication side effects. If a new medication coincides with the onset of a burning sensation, discuss it with a doctor. The doctor can assess if the medication is the cause. They can also suggest alternatives or adjustments. This helps manage the pain or sensation.
Neurological Causes of Burning Sensation
A burning sensation in the head can often come from issues with the body’s nerves. These problems can cause nerve irritation or damage. When nerves do not work correctly, they send unusual signals. The brain interprets these signals as a burning feeling or other strange sensations.
Nerve Compression or Damage
Nerves can become squeezed or hurt in different parts of the body. This compression or damage can lead to a burning feeling. For example, cervical spondylosis is a condition where neck bones wear down. This can press on nerves in the neck.
This pressure causes burning pain in the neck or shoulders. This pain can even spread to the head or scalp. Sometimes, a squeezed nerve root, called radicular compression, causes an itchy feeling on the scalp. This feeling includes burning, tingling, and itching. The occipital nerves are located in the scalp. Injury or inflammation of these nerves can cause burning pain. This pain appears in the upper neck, the back of the head, or behind the ears. These nerves come from the upper spinal nerve roots in the neck.
Neuropathy and Neuralgia
Neuropathy refers to damage to the peripheral nerves. These nerves carry messages between the brain, spinal cord, and the rest of the body. When these nerves are damaged, they can send wrong signals.
This causes a burning sensation, numbness, or tingling. Peripheral neuropathy specifically affects nerves outside the brain and spinal cord. Neuralgia describes severe pain along the path of a nerve. Both conditions involve nerve problems that lead to uncomfortable sensations.
Occipital Neuralgia and Small Fiber Neuropathy
Occipital neuralgia is a specific type of headache. It involves the occipital nerves. People with this condition often feel a throbbing or burning pain. This pain starts at the base of the skull and spreads to the scalp. Small fiber neuropathy affects the small nerve fibers in the skin.
These fibers control pain and temperature sensations. When these small nerves are damaged, they can cause intense burning, tingling, or electric-shock-like pain. This burning can occur anywhere on the body, including the head.
Post-Concussion Syndrome
A concussion is a type of brain injury. Post-concussion syndrome happens when symptoms last for weeks or months after the initial injury. People with this syndrome can experience various symptoms.
These include headaches, dizziness, and difficulty concentrating. Some also report a burning feeling in their head. This sensation comes from changes in how the brain processes sensory information after the injury.
Seizure Disorders
Seizure disorders involve unusual electrical activity in the brain. While many people think of seizures as convulsions, they can also cause sensory symptoms. Seizures starting in the parietal lobe of the brain can cause sensations of burning, cold, or pain.
Other symptoms from these seizures include numbness, tingling, prickling, crawling, or electric-shock sensations. A focal sensory seizure is a type of seizure. It causes a sensation without other clear physical signs. These seizures can include a “cephalic sensation.” This is a feeling in the head like light-headedness or a headache. These sensations are a type of epileptic “aura.” An aura is a subjective experience.
It shows the start of a seizure. An aura can be the only symptom or can lead to other seizure types. It is important to know that some seizure symptoms might hide other minor signs. Therefore, a patient experiencing only one type of symptom does not mean other seizure activities are not happening in other brain areas.
Serious Medical Conditions and Brain Inflammation
A “brain burning feeling” can sometimes signal more serious underlying medical conditions. These conditions often involve inflammation within the brain. Brain inflammation may not always present as typical pain. Instead, it can reduce normal brain functions. This can lead to a range of unusual sensations and cognitive difficulties, including brain fog.
Brain Inflammation
Brain inflammation, also known as encephalitis, occurs when the brain’s tissues swell. This swelling can result from infections, autoimmune responses, or other injuries. When the brain experiences inflammation, its delicate nerve pathways can become irritated or damaged.
This irritation can lead to a burning sensation. It can also cause other neurological symptoms. These symptoms include headaches, confusion, and brain fog. Recognizing the signs of brain inflammation is crucial. Early diagnosis allows for timely intervention. This can help prevent further damage. Lifestyle choices and managing underlying conditions can help prevent brain inflammation. Seeking appropriate medical care is the best way to address and potentially find treatment for brain inflammation.
Autoimmune Encephalitis
Autoimmune encephalitis is a condition where the body’s immune system mistakenly attacks healthy brain cells. This attack causes significant brain inflammation.
The immune system produces antibodies that target specific proteins in the brain. This leads to a variety of neurological and psychiatric symptoms. These symptoms can include seizures, memory problems, confusion, and personality changes. Patients often report a persistent brain fog. They might also experience unusual sensations like a burning feeling in the head. Diagnosing autoimmune encephalitis can be complex.
Doctors often use blood tests, spinal fluid analysis, and MRI scans. Early diagnosis and treatment are vital. They can significantly improve outcomes for individuals with autoimmune encephalitis.
Vasculitis Affecting the Brain
Vasculitis involves inflammation of blood vessels. When vasculitis affects the brain, it can lead to serious neurological problems. Primary Angiitis of the Central Nervous System (PACNS) is a rare form of vasculitis. It specifically targets blood vessels in the brain and spinal cord. Diagnosing isolated CNS vasculitis presents challenges.
Symptoms like headache and brain fog are non-specific. The condition can mimic infections or tumors. Imaging techniques like MRI and cerebral angiography can sometimes give misleading results. A brain biopsy is often necessary for a definitive diagnosis. However, even a negative biopsy does not completely rule out the condition.
The diagnostic criteria for PACNS include:
An unexplained neurologic deficit after thorough clinical and laboratory evaluation.
Evidence of an arteritic process confirmed by cerebral angiography or tissue examination.
No indication of systemic vasculitis or any other condition that could explain the angiographic or pathologic findings.
While PACNS directly affects the brain, other forms of vasculitis can impact peripheral nerves.
Non-systemic vasculitic neuropathy (NSVN) affects nerves outside the brain. Pure sensory involvement, including burning sensations, occurs in up to 15% of NSVN cases. This condition typically involves both sensory and motor peripheral nerves. It often presents as mononeuritis multiplex. This means asymmetric dysesthesias, paresthesias, and palsies affect two or more individual peripheral nerves.
Multiple Sclerosis
Multiple Sclerosis (MS) is a chronic disease. It affects the brain and spinal cord. In MS, the immune system attacks the myelin sheath. Myelin is the protective covering of nerve fibers. This attack causes brain inflammation and nerve damage. This damage disrupts communication between the brain and the rest of the body.
Symptoms vary widely. They can include numbness, tingling, muscle weakness, vision problems, and fatigue. Many individuals with MS report unusual sensory experiences. These experiences include a burning sensation in the head or other body parts.
They also often experience brain fog. The exact cause of MS is unknown. However, researchers believe a combination of genetic and environmental factors plays a role. Managing MS often involves medications to slow disease progression and manage symptoms.
Temporal Arteritis
Temporal arteritis, also known as giant cell arteritis, is a serious inflammatory condition. It affects the arteries, especially those in the head and neck. This condition causes inflammation and damage to the blood vessel walls. This can lead to reduced blood flow.
The most common manifestation is a new onset of headache. This headache is often severe and localized to the temples. Patients frequently report scalp tenderness. They might also experience jaw claudication, which is pain in the jaw when chewing. A burning feeling in the head can also occur due to the inflamed arteries.
The American College of Rheumatology criteria for diagnosing temporal arteritis include:
Age over 50 years at onset.
New onset of headache.
Elevated Erythrocyte Sedimentation Rate (ESR) greater than 50 mm/h.
Abnormal temporal artery (tenderness or reduced pulsation).
An abnormal arterial biopsy confirming temporal arteritis.
Specific diagnostic tests for temporal arteritis include:
Temporal Artery Biopsy: This is the gold standard for diagnosis. Doctors recommend a minimum 2-cm biopsy. A negative biopsy does not rule out the diagnosis.
Acute Phase Reactants: Elevated levels of ESR, C-reactive protein (CRP), and interleukin-6 may be present. A CRP over 2.45 mg/dL and platelet count over 400,000 strongly predict a positive biopsy.
Duplex Ultrasonography: This can show vessel wall thickening, known as a ‘halo sign.’
Fluorescein Angiography: This may reveal prolonged choroidal and central retinal artery filling times.
Temporal arteritis can present in three ways: cranial arteritis, extracranial arteritis, and polymyalgia syndrome.
The most severe complication is arteritic anterior ischemic optic neuropathy (AAION). This leads to sudden, painless, profound vision loss. Early diagnosis and treatment with corticosteroids are crucial. They help prevent permanent vision loss and other complications affecting the brain.
Other Potential Contributors
A burning feeling in the brain can also stem from other factors. These factors include hormonal shifts, lack of nutrients, and stopping certain substances.
Hormonal Fluctuations
Hormones play a large role in brain function. Changes in hormone levels can cause various neurological sensations. Many women experience migraines linked to their menstrual cycle.
Up to 25% of women report this connection. Lower levels of progesterone and estrogen during the late luteal phase can increase migraine risk. This happens by activating the internal opioid system.
Some women experience more migraine activity during the first three days of their period. This also occurs about two days before menstruation. After puberty, migraines are twice as common in women than men. This links to reproductive events with changing estrogen levels. These events include pregnancy and perimenopause. Hormonal migraines can occur when estrogen levels fluctuate or drop.
Estrogen directly influences neurotransmitters in the migraine pain pathway. High estrogen can increase glutamate activity and migraine auras. A drop in estrogen and changes in serotonin receptors can trigger migraines. Estrogen may cause menstrual migraines by acting on the trigeminovascular system.
It relaxes blood vessel muscles, dilates them, and increases blood flow to the brain. This sensitizes pain-causing nerves. Hormonal changes can affect migraines around pregnancy, birth, hormone replacement therapy, and contraception. They also affect menstruation, perimenopause, and menopause.
During perimenopause, estradiol levels can be much higher or lower. Other hormones like progesterone also change. These drastic hormone fluctuations affect key brain functions.
They lead to symptoms such as hot flashes, mood changes, sleep problems, and cognitive issues. The pre-frontal cortex is affected by estradiol changes. This leads to cognitive symptoms resembling ADHD. Women also report challenges with executive functioning skills.
There is a two-fold greater risk for depression during menopause. Hot flashes and night sweats can disrupt sleep. This leads to daytime cognitive and mood challenges, adding to overall stress. The symptoms of perimenopause are largely neurological. They include temperature dysregulation, depression, insomnia, pain, and cognitive dysfunction. This can cause significant stress.
Nutritional Deficiencies
The brain needs specific nutrients to work correctly. A lack of these nutrients can lead to nerve damage. This damage causes unusual sensations. Deficiencies in copper, vitamins B1, B6, B9 (folic acid), B12, and E are most likely to cause nerve damage.
Neuropathy symptoms include pain, numbness, and tingling in hands or feet. A deficiency in alpha-tocopherol (a type of vitamin E) also links to neuropathy. Vitamin B12 deficiency can damage the myelin sheath. This leads to symptoms like pain, numbness, and ‘pins and needles’ sensations. Too much vitamin B6 can also lead to nerve damage. These deficiencies can contribute to a brain burning feeling and overall brain fog.
Substance Withdrawal
Stopping certain substances can cause the body to react strongly. This reaction often includes neurological symptoms. When someone stops using alcohol, caffeine, or certain medications, withdrawal symptoms can appear.
These symptoms can include headaches, dizziness, and a burning sensation in the head. The body experiences stress as it adjusts to the absence of the substance. This stress can manifest as physical discomfort. This discomfort includes a burning feeling. It can also cause brain fog.
Diagnosing a Brain Burning Feeling
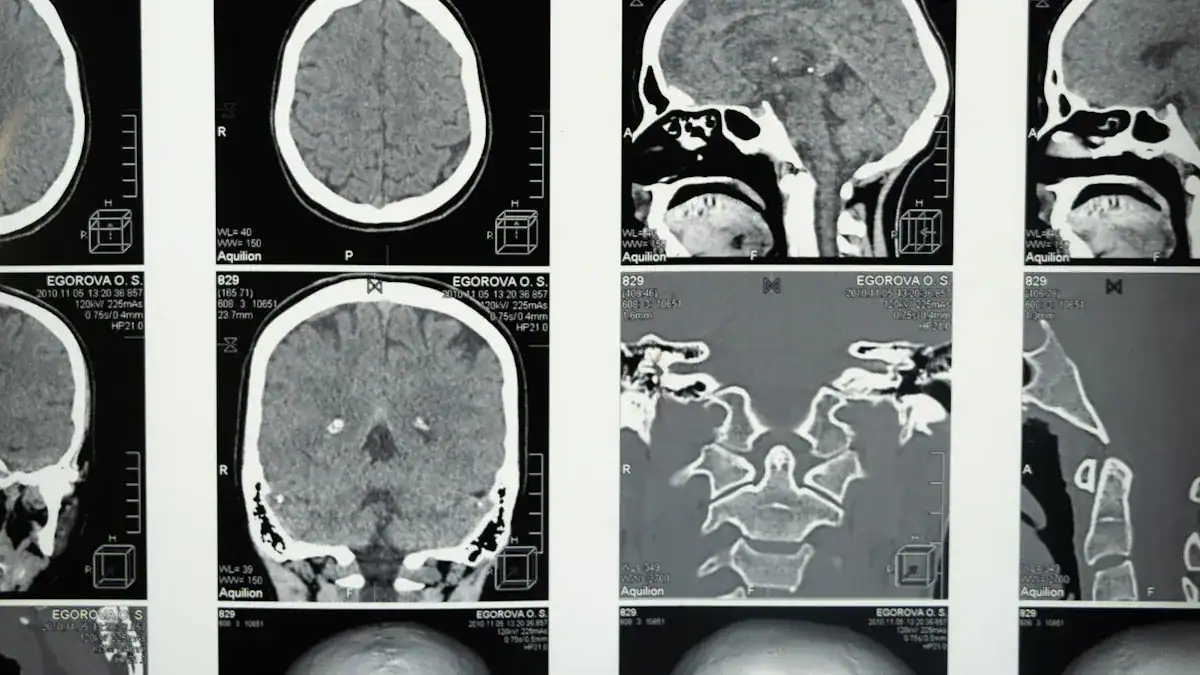
Understanding the cause of a brain burning feeling requires careful investigation. Doctors use various methods to pinpoint the underlying issue. This process often involves several steps, from initial consultation to specialized diagnostic testing.
Initial Medical Consultation
A doctor begins the diagnosis process with an initial medical consultation. They examine the patient’s medical history. This includes past illnesses, medications, and any relevant family history. The doctor then performs a physical and neurological examination.
This helps assess overall health and nerve function. Based on these findings, the doctor may recommend further diagnostic testing. These tests include EMG, nerve conduction studies, or imaging scans to determine the underlying cause of the brain burning feeling.
Neurological Examination
During a neurological examination, the doctor assesses the patient’s mental status, coordination, reflexes, and sensory responses. They check for any signs of nerve damage or dysfunction.
This examination helps identify which nerves might be affected. It also guides further investigation into potential brain inflammation or other neurological conditions.
Imaging Tests: MRI and CT Scans
Imaging tests like MRI and CT scans are crucial for visualizing the brain and surrounding structures. MRI of the brain is a primary tool for assessing and differentiating suspected neurological conditions. These conditions include Alzheimer’s Disease and Vascular Dementia. MRI can help rule out neurodegenerative disorders.
It also screens for various chronic orofacial pain types. This excludes structural issues such as intracranial tumors, cysts, or trigeminal nerve vascular compression. A study of 125 patients showed intracranial pathologies in 48.8%. These included trigeminal neurovascular contact, cerebral small vessel disease, and space-occupying lesions. These scans help identify structural problems or signs of brain inflammation that could cause the burning sensation.
Blood Tests and Lab Work
Doctors often order blood tests to check for various conditions. These tests can identify infections, autoimmune markers, or nutritional deficiencies. For example, blood tests can reveal signs of brain inflammation or systemic issues affecting nerve health.
Nerve Conduction Studies
Nerve conduction studies measure how fast electrical signals travel through nerves. These tests help identify nerve damage or compression. They can pinpoint specific nerves causing the brain burning feeling. This diagnostic testing is vital for understanding nerve function.
Lumbar Puncture
A lumbar puncture, or spinal tap, involves collecting cerebrospinal fluid (CSF). Doctors analyze this fluid for signs of infection, brain inflammation, or other neurological diseases. This procedure provides direct insight into the central nervous system’s health.
When to Worry and Seek Medical Attention
A “brain burning feeling” can sometimes signal a serious health issue. People should know when to seek medical help. Certain signs indicate a need for immediate medical evaluation.
Sudden Onset and Severe Pain
A sudden onset of a burning sensation in the head requires attention. If the burning feeling appears very quickly and is intense, it is a red flag. Severe pain that comes on without warning needs prompt medical assessment. This type of sudden, intense discomfort can indicate an acute problem. Do not ignore such symptoms.
Accompanied by Neurological Symptoms
A burning sensation becomes more concerning when other neurological symptoms appear.
These symptoms include weakness in an arm or leg. Vision changes, such as blurred vision or double vision, are also serious. Difficulty speaking or understanding speech is another critical sign. Numbness or tingling on one side of the body also warrants immediate medical attention. These combined symptoms suggest a potential issue with the brain or nervous system.
Persistent or Worsening Sensation
A burning sensation that does not go away or gets worse over time needs medical evaluation. A persistent burning sensation indicates an ongoing problem. Doctors recommend electrodiagnostic studies if symptoms are concerning.
These concerns include acute onset, asymmetrical symptoms, or rapidly progressive clinical course. Urgent referral to a neurologist is advised for acute, subacute, severe, or progressive symptoms. This prevents delays in treatment. For conditions like “brain on fire disease,” symptoms typically begin mildly. They then rapidly worsen to a point requiring hospitalization. This rapid progression of burning pain is a serious indicator.
Following Head Trauma
Any burning feeling in the head after a head injury is a cause for concern. Even a mild bump to the head can sometimes lead to unexpected symptoms. A burning sensation after head trauma could indicate a concussion or other brain injury. It is important to get checked by a doctor. They can assess the injury and prevent further complications.




