
The ability to move relies on a healthy muscular system, yet its impairment significantly impacts daily well-being for billions worldwide. In 2020, musculoskeletal disorders affected over 1.63 billion people globally, highlighting their widespread impact.
Muscular system diseases are a broad category of conditions that affect muscle function, strength, and structure, often leading to muscular weakness, pain, or paralysis. This blog provides clear, factual information on the causes, diverse symptoms, and key facts about these conditions, empowering readers with essential knowledge.
Key Takeaways
Muscular system diseases affect muscle function. They cause weakness, pain, or paralysis. Over 1.6 billion people worldwide have these conditions.
These diseases have many causes. They include genes, immune system attacks, injuries, infections, and poor nutrition. Understanding the cause helps with treatment.
Common symptoms include muscle weakness, pain, and tiredness. Some people have trouble moving or coordinating. Specific signs like drooping eyelids can also appear.
Doctors use many tests to find these diseases. These tests include blood work, MRI scans, and muscle biopsies. Early diagnosis helps a lot.
Treatment focuses on managing symptoms. It also aims to improve life quality. This includes medicines, physical therapy, and lifestyle changes.
Causes of Muscular System Diseases
Muscular system diseases arise from various origins. Understanding these causes helps clarify the nature of these complex conditions.
Genetic and Inherited Factors
Many muscular system diseases originate from genetic and inherited factors. These conditions occur when changes happen in a person’s genes. These genetic changes often affect proteins essential for healthy muscle structure and function. For example, muscular dystrophy results from mutations in genes. These mutations prevent cells from properly maintaining muscles, leading to progressive muscle weakness. Many different forms of muscular dystrophy exist because numerous genes and potential genetic mutations are involved in muscle function.
Duchenne muscular dystrophy (DMD) and Becker muscular dystrophy (BMD) both stem from changes in the same gene. While they share similar symptoms, DMD is more severe and progresses more rapidly than BMD. Specifically, Duchenne muscular dystrophy (DMD) is a progressive, genetic (X-linked recessive) neuromuscular disorder.
Mutations in the DMD gene cause it. These mutations lead to the dysfunction or absence of the dystrophin protein. Dystrophin is crucial for maintaining muscle cell integrity. Without functional dystrophin, muscle cells become vulnerable to injury, resulting in progressive muscle degeneration and weakness. Becker muscular dystrophy (BMD) is a milder condition also classified as a dystrophinopathy.
Genetic muscular disorders can be inherited in several ways. In autosomal dominant inheritance, having one copy of the disease-causing gene leads to symptoms. A person has a 50% chance of passing it to each child. Examples include Myotonic dystrophy (DM), facioscapulohumeral muscular dystrophy (FSHD), and some types of limb-girdle muscular dystrophy (LGMD1). Autosomal recessive conditions require two copies of the mutated gene for symptoms to appear. Individuals with one copy are carriers.
If both parents are carriers, each child has a 25% chance of having the condition. Examples include most types of spinal muscular atrophy (SMA), most types of congenital muscular dystrophy (CMD), and limb-girdle muscular dystrophy type 2 (LGMD2). X-linked recessive inheritance is another pattern for some disorders. Duchenne muscular dystrophy (DMD) and Becker muscular dystrophy (BMD) follow an X-linked recessive pattern. The mutated gene is on the X chromosome. Males only need one mutated X chromosome to be affected. Females need both X chromosomes to carry the mutation to be affected.
Autoimmune and Inflammatory Conditions
Autoimmune and inflammatory conditions occur when the body’s immune system mistakenly attacks its own healthy tissues, including muscles. This attack leads to inflammation and damage. Dermatomyositis (DM) is a rare autoimmune disease. It attacks the muscles, causing inflammation and damage. It belongs to a group of conditions called Idiopathic Inflammatory Myopathies (IIM). In IIM, the body produces antibodies that attack muscles and other connective tissue. Immune-mediated necrotizing myopathy (IMNM) is one of the three most common subgroups of IIM. Anti-synthetase syndrome (ASyS) is another common subgroup of IIM.
Doctors often look for specific inflammatory markers in the blood to diagnose these conditions. Creatine Kinase (CK) levels are often significantly increased. They can range from 10- to 50-fold above normal. This is especially high in necrotizing autoimmune myopathy (NAM).
In early, active stages, CK can exceed 50 times the upper limit of normal (ULN). However, CK levels can be normal in cases with less muscle necrosis or advanced muscle wasting. Serum concentrations of Aspartate Transaminase (AST), Alanine Transaminase (ALT), and Lactate Dehydrogenase (LDH) above the ULN can also support a diagnosis of inflammatory myopathies. Antinuclear Antibodies (ANAs) and Myositis-related Antibodies are also included in laboratory testing for inflammatory myopathies.
Injury, Trauma, and Overuse
Physical injuries, trauma, and overuse can directly damage muscles and lead to muscular problems. Injuries that do not heal properly often cause chronic musculoskeletal pain. While injuries frequently cause acute pain, their improper healing can result in long-term conditions affecting the muscular system. Repetitive strain injury (RSI) is a common issue.
It develops from repeated movements or sustained awkward postures. Untreated repetitive strain injury (RSI) can lead to chronic pain. It can also result in long-term disability. Excessive repetitive motion wears down cartilage. It also tightens muscles and reduces flexibility. These effects increase the risk of chronic pain or muscle strain.
Infections and Environmental Triggers
Infections and exposure to certain environmental triggers can also cause muscular system diseases. Various viruses and bacteria can cause muscle damage. Viruses include Influenza A and B, parainfluenza viruses, adenoviruses, respiratory syncytial viruses, arboviruses (including Chikungunya and Dengue), Mumps, parvovirus B19, and Covid-19. Bacteria include Staphylococcus aureus, gram-positive, gram-negative, anaerobic, mycobacterial, and atypical bacteria.
Myositis can be caused by systemic infections, particularly viral infections like influenza. Parasitic infections, such as trichinosis from undercooked meat, can also lead to muscle invasion. Pyomyositis is a specific type of infectious myositis. It is a bacterial infection often caused by Staphylococcus bacteria. It results in pus-filled abscesses within muscles.
Environmental toxins also affect muscle function. These toxins interfere with the neuromuscular apparatus. They interfere with voltage-gated ion channels. They disrupt acetylcholine release. They affect depolarization of the postsynaptic membrane.
They impact the generation and spread of the muscle action potential. Environmental toxins known to affect muscle function include plant poisons, such as curare. Bacterial poisons, such as botulinum toxin, also cause problems. Animal toxins include venoms from snakes and arthropods, venoms from certain marine creatures, skin secretions from dart-poison frogs, and toxins from poisonous fish, shellfish, and crabs.
Metabolic and Nutritional Deficiencies
Metabolic and nutritional deficiencies impact how muscles produce and use energy. Metabolic myopathies are rare disorders. They disrupt energy metabolism, primarily affecting skeletal muscle due to its high energy demand. Understanding these disorders requires knowledge of the biochemical pathways involved in energy production during rest, exercise, and stress. Adenosine triphosphate (ATP) is the primary energy source for muscle contraction. While fatty acids are the main fuel at rest, exercise activates various pathways. These include anaerobic glycolysis for high-intensity bursts and oxidative phosphorylation for sustained activity. These pathways utilize glycogen, glucose, and fatty acids. Metabolic myopathies arise from defects in any of these energy production pathways.
Metabolic myopathies are disorders of muscle energy production. They lead to skeletal muscle dysfunction. These conditions can also involve cardiac and systemic metabolic dysfunction. Symptoms are often intermittent. Exercise or changes in the availability of lipid and carbohydrate fuels trigger them.
These disorders are organized into three major groups: glycogen metabolism disorders, lipid metabolism disorders, and mitochondrial myopathies. Glycogen metabolism disorders impair the body’s ability to convert glucose stores into usable energy. They primarily affect the liver and skeletal muscle.
Lipid metabolism disorders impair the ability to break down fatty acids for energy production. This leads to muscle weakness and pain during prolonged exercise. Mitochondrial myopathies result from dysfunction in mitochondria. Mitochondria are the primary sites of energy production within cells. These myopathies affect the musculoskeletal system among others.
Nutritional deficiencies also impair muscle metabolism. Inadequate dietary intake of energy and protein leads to the catabolism of body fat and muscles to provide energy substrates. This results in metabolic dyshomeostasis and fatigue. A maternal low-protein diet during lactation has been shown to reduce muscle mass and strength in offspring. This effect is more pronounced in males. Nutritional biomarkers such as albumin and iron are linked to musculoskeletal health. Deficiencies in these could impair muscle metabolism.
Types of Muscular System Diseases: Symptoms & Facts
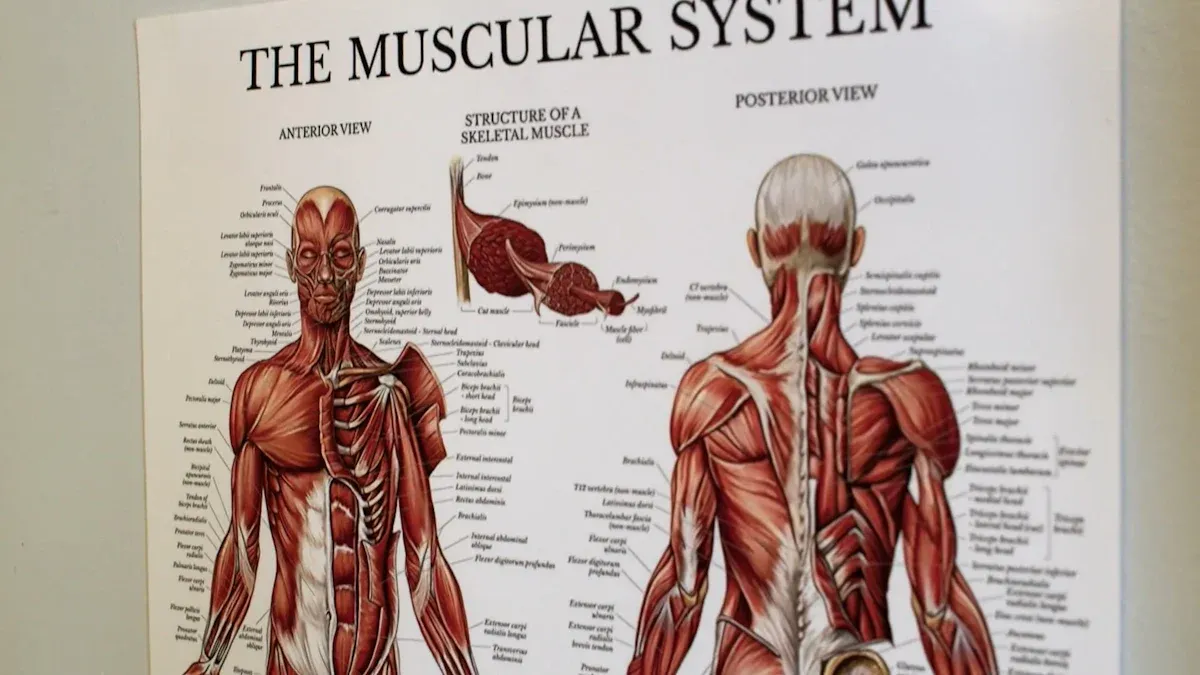
Muscular system diseases encompass a wide range of conditions. Each condition has unique characteristics, specific causes, detailed symptoms, diagnostic methods, and treatment options. Symptoms vary depending on the specific type of disease.
Muscular Dystrophy
Muscular dystrophy refers to a group of genetic disorders. These disorders cause progressive muscle weakness and loss of muscle mass. Genetic changes affect proteins essential for healthy muscle formation. This leads to progressive muscle weakness. Numerous types of muscular dystrophy exist. Duchenne Muscular Dystrophy (DMD) is one type. It typically begins in early childhood, around ages 2-3, and primarily affects boys.
Doctors diagnose muscular dystrophy through several methods. A complete medical history and physical examination are essential. This includes a family history review. Electrodiagnostic tests, such as electromyography (EMG) and nerve conduction studies (NCS), assess muscle and nerve function. Laboratory tests check muscle enzymes and other diagnostic clues. Muscle biopsy provides a microscopic examination of muscle tissue. Imaging studies, like CT and MRI, detect abnormalities in organs and scoliosis. An electrocardiogram (ECG) checks heart rhythm.
Specific diagnostic tools for muscular dystrophy include Creatine Kinase (CK) levels. Blood tests measure CK, a muscle enzyme that leaks from damaged muscle. Very high CK levels, 10 to 20 times the upper limit of normal, indicate muscular dystrophy. These levels peak around age 2 and then gradually decrease. Genetic testing is crucial for confirming the diagnosis. It analyzes DNA, usually from blood cells, to identify mutations in the DMD gene. This often starts with large deletion/duplication mutations.
Doctors use next-generation sequencing if initial results are negative. Cardiac monitoring is essential due to common DMD-associated cardiomyopathy. It includes electrocardiogram (ECG), echocardiography, or cardiac MRI. These detect conduction abnormalities, structural changes, and fibrotic scarring. Pulmonary monitoring involves regular assessment of respiratory muscle strength. Doctors use pulmonary function tests to guide interventions and prevent breathing complications. Sleep studies, like polysomnography, may detect sleep apnea.
The progression of muscular dystrophy varies greatly among its types. Some types of muscular dystrophy show rapid progression, while others progress slowly. Treatment focuses on managing symptoms and improving quality of life.
Myasthenia Gravis
Myasthenia gravis is an autoimmune neuromuscular disorder. It affects communication between nerves and muscles. This leads to fluctuating muscle weakness. The immune system mistakenly attacks healthy tissues at the neuromuscular junction. This disrupts the signals from nerves to muscles.
Common symptoms of myasthenia gravis include drooping eyelids (ptosis), double vision (diplopia), and difficulty swallowing (dysphagia). Patients may also experience general muscle weakness that worsens with activity and improves with rest. The weakness can affect facial muscles, making expressions difficult. It can also affect limb muscles, causing problems with walking or lifting.
Treatment for myasthenia gravis is tailored to disease severity and subtype. Acetylcholinesterase inhibitors, such as Mestinon® (pyridostigmine bromide) and Regonol® (pyridostigmine bromide), improve nerve-to-muscle communication. Corticosteroids and other immunosuppressants, like CellCept® (mycophenolate mofetil), Cyclosporin, Imuran® (azathioprine), and Prednisone, reduce the immune system’s attack. Thymectomy, the surgical removal of the thymus gland, is also a treatment option.
Neuromuscular Diseases
Neuromuscular diseases are a broad category. They involve dysfunction of peripheral nerves, muscles, or their communication. These conditions can cause muscle weakness or paralysis even when the nervous system is intact. This means the problem lies within the muscle itself or the connection point. Neuromuscular diseases include conditions like muscular dystrophy, myasthenia gravis, and motor neuron diseases.
Symptoms often include muscle weakness and wasting. Patients may experience fatigue, muscle cramps, and difficulty with movement. The specific symptoms depend on the affected nerves and muscles. Diagnosis involves neurological exams, electrodiagnostic tests, and sometimes muscle biopsies. Treatment focuses on managing symptoms and slowing disease progression.
Fibromyalgia
Fibromyalgia is a chronic disorder. It causes widespread pain and tenderness throughout the body. It also causes fatigue, sleep problems, and cognitive difficulties. The exact cause of fibromyalgia is unknown. However, current theories suggest several contributing factors.
Abnormal pain signaling pathways play a role. Genetic predisposition can increase risk. Abnormal neuroendocrine and autonomic system activity also contributes. Environmental triggers and sleep disturbances are common. Fibromyalgia also connects to affective spectrum disorders (ASD). Some research suggests a potential role of small fiber neuropathies.
Other theories point to central augmentation of sensory input. Impaired central cortical processing and dysregulation of the central nervous system at the spinal cord level are also considered. Reductions in neurotransmitters, such as serotonin, are observed. Hyperactivity of the HPA axis and abnormalities in the autonomic nervous system also occur.
Decreased opioid release and alteration in serotonin and noradrenergic secretion are seen in chronic pain states. Oxidative stress and maladaptive immune responses may also contribute. Psychological stressors, physical trauma, and vitamin deficiencies, such as thiamine deficiency, can also trigger or worsen fibromyalgia symptoms.
Fibromyalgia symptoms include widespread pain, often described as a constant dull ache. Fatigue is common, ranging from mild to severe. Sleep disturbances, such as insomnia or restless leg syndrome, are frequent. Cognitive difficulties, sometimes called “fibro fog,” include problems with memory and concentration. Treatment involves medication, lifestyle changes, and therapies like exercise and stress reduction.
Tendinitis and Bursitis
Tendinitis and bursitis are common inflammatory conditions. They affect the musculoskeletal system. Tendinitis is the inflammation of a tendon. Tendons are thick cords that attach muscle to bone. Bursitis is the inflammation of a bursa. Bursae are small, fluid-filled sacs that cushion bones, tendons, and muscles near joints.
Common causes include repetitive overuse. Frequent, repeated movements can strain tendons and hinder proper healing. Aging and wear-and-tear also contribute. Tendons naturally lose elasticity and weaken over time, increasing susceptibility to injury. Poor biomechanics, such as incorrect movement patterns or muscle imbalances, can lead to chronic tendon stress. Lack of recovery, meaning insufficient rest between physical activities, can also cause chronic issues. A sudden increase in activity without proper conditioning can overload tendons.
Risk factors for chronic tendinitis include repetitive activities common in gardening, landscaping, woodworking, shoveling, painting, scrubbing, or sports like tennis, golf, or baseball. Poor posture can contribute to tendon stress. Certain medical conditions that weaken muscles also increase risk.
Age is a significant factor; after 40, tendons become less elastic, tolerate less stress, and tear more easily. Being over 60 is a specific risk factor. Being overweight also increases risk. Underlying conditions like rheumatoid arthritis, gout, and type 2 diabetes are risk factors. A sedentary lifestyle can also contribute.
Symptoms of tendinitis and bursitis include pain, tenderness, and stiffness near the affected joint. The pain often worsens with movement or activity. Swelling and redness may also be present. Diagnosis typically involves a physical examination and imaging tests like ultrasound or MRI. Treatment often includes rest, ice, pain relievers, and physical therapy.
Rhabdomyolysis
Rhabdomyolysis is a serious medical condition. It occurs when damaged muscle fibers release their contents into the bloodstream. These contents, including myoglobin, can harm the kidneys and cause kidney failure.
Common causes of rhabdomyolysis include injury or trauma. Severe burns, electrocution, or crushing injuries are among the most common causes. High-intensity exercise, especially starting an exercise program too quickly without adequate muscle recovery, can also trigger it. Severe dehydration and overheating accelerate muscle breakdown.
Dehydration impairs kidney function to remove waste. Medications, such as antipsychotic, antidepressant, antiviral, and statin medications, especially when treating diabetes or liver disease, can cause rhabdomyolysis. Substance use disorder, involving non-prescribed psychoactive drugs, can lead to muscle deterioration. Long periods of inactivity, such as falling and being unable to get up for an extended time, are also causes. Certain medical conditions, like genetic conditions such as McArdle disease and Duchenne muscular dystrophy, as well as metabolic or mitochondrial conditions, can also cause rhabdomyolysis.
Other causes include crush injuries from vehicle accidents or other severe trauma. Heatstroke can also cause it. Bites from certain venomous snakes can lead to severe muscle damage.
In adults, drug or alcohol abuse, medicinal drug use, trauma, neuroleptic malignant syndrome (NMS), and immobility are common causes. In the pediatric population, viral myositis, trauma, connective tissue disorders, exercise, and drug overdose are frequent causes. Viral myositis alone can account for up to one-third of cases in children.
Blunt and crush injuries are common causes of trauma-induced rhabdomyolysis. This is particularly true when acute compression of muscle is relieved, allowing breakdown products to enter circulation. High-voltage electrical injuries, such as electrocution or lightning strikes, also contribute. Up to 10% of survivors develop rhabdomyolysis.
Exertional rhabdomyolysis can occur after strenuous exercise. Increased temperature and humidity potentially play a role. Heat stroke, defined as a core body temperature exceeding 40.5°C, can lead to rhabdomyolysis along with other severe complications. Neuroleptic malignant syndrome (NMS), often linked to antipsychotic medications, causes rhabdomyolysis due to massive heat generation from rigidity and tremor. This likely stems from central nervous system dopamine receptor blockade or withdrawal of dopaminergic agonists.
Symptoms include severe muscle pain, weakness, and dark, reddish-brown urine. Diagnosis involves blood tests to check for elevated CK levels and myoglobin. Treatment focuses on preventing kidney damage through intravenous fluids and addressing the underlying cause.
General Symptoms of Muscular System Diseases

Muscular system diseases present a range of common indicators. These symptoms can vary widely among different conditions. However, several general signs often point to underlying muscular issues.
Muscle Weakness and Fatigue
A primary symptom of many muscular system diseases is muscle weakness. This weakness can affect all muscle groups. Specific disorders may initially affect the face, feet, hands, and neck. Doctors use objective measures to quantify muscle weakness. These include dynamometers, modified sphygmomanometers, and vigorometers. The Childhood Myositis Assessment Scale also helps evaluate strength. Patients often experience significant fatigue, which worsens with activity.
Pain, Stiffness, and Cramps
Many individuals with muscular conditions experience muscle pain, stiffness, and cramps. These can be signs of certain musculoskeletal system diseases or neuromuscular disorders. Inflammatory myopathies, for example, cause chronic muscle inflammation and weakness.
Some patients with inflammatory myopathy may experience slight muscle pain or muscles that are tender to the touch. Muscle pain is not a common symptom in dermatomyositis, but it can occur, especially when the fascia is involved. Anti-SRP-IMNM is frequently associated with myalgia. Delayed muscle relaxation after contraction can also occur.
Impaired Movement and Coordination
Muscular system diseases often lead to impaired movement and coordination. Patients may struggle with fine motor skills or balance. Neurological tests assess these impairments. The finger-to-nose and finger-to-finger tests check coordination. Patients extend their arm and touch their nose or an examiner’s finger. Difficulty is called dysmetria. Rapid alternating movements, like quickly flipping one hand back and forth, assess dysdiadochokinesia. Electromyography (EMG) evaluates muscle and nerve function. Nerve conduction tests assess peripheral nerve function.
Specific Manifestations: Drooping Eyelids, Double Vision, Difficulty Swallowing
Certain muscular conditions show very specific symptoms. Drooping eyelids (ptosis) and double vision (diplopia) are common initial symptoms of Myasthenia Gravis. This condition weakens muscles controlling eye movement and eyelids. Patients also often report difficulty swallowing (dysphagia). These specific manifestations help doctors diagnose particular muscular disorders.
Muscle Atrophy or Enlargement
Muscular system diseases can cause changes in muscle size. Muscle atrophy refers to muscle wasting or shrinking. Conditions like lower motor neuron pathology, frailty, sarcopenia, and hypothyroidism can cause muscle atrophy. Becker muscular dystrophy causes atrophy in the hips, proximal legs, and arms. Myotonic dystrophy type 1 leads to distal atrophy and wasting in facial muscles. Conversely, some conditions can cause muscle enlargement, though this is less common.
Diagnosis and Treatment for Muscular System Diseases
Doctors use various methods to identify and manage muscular system diseases. Early and accurate diagnosis is crucial for effective treatment.
Diagnostic Methods and Tools
Diagnosing muscular system diseases involves several steps. A physical exam helps identify muscular signs and checks other organs. Blood tests measure muscle enzymes like CK, LDH, and aldolase. High levels of these enzymes often indicate muscle damage.
An electromyogram (EMG) studies the electrical activity of nerves and muscles. This assesses their function. MRI is an imaging technique. It evaluates muscles for inflammation, atrophy, and specific involvement patterns. MRI also guides biopsies. An Ischaemic Forearm Test assesses the muscle’s ability to generate energy from glucose. It measures lactate and ammonium levels during exercise. Muscle and nerve biopsies are invasive procedures. They confirm diagnoses or guide genetic studies. Genetic studies identify inherited conditions.
Biomarkers also help in diagnosis and monitoring. TNF-α is a protein that mediates inflammation. It relates to Duchenne Muscular Dystrophy (DMD) progression.
Increased concentrations appear in affected muscles. Other biomarkers include Skeletal Troponin I (sTnI), Myosin Light Chain 3 (Myl3), Creatine Kinase (CK), Creatine Kinase Muscle-type (CKM), and Fatty Acid Binding Protein 3 (FABP3). These are often elevated in muscular dystrophy patients.
Physical Therapy and Rehabilitation
Physical therapy plays a vital role in managing muscular conditions. It helps improve muscle strength and function. Aerobic moderate-intensity exercise, like cycling, improves oxidative capacity and muscle function.
Submaximal and aerobic functional exercises, such as swimming, optimize strength. Low-intensity aerobic endurance training improves VO2max and physical endurance. Low-intensity resistance training increases muscle maximal strength and endurance. Supervised low-load resistance training is well tolerated. It improves strength and endurance without causing muscle damage.
Assistive technologies also support individuals. Mobility devices include manual and power wheelchairs. Orthotic supports like ankle-foot orthoses prevent contractures. Communication aids, such as eye-tracking devices and voice recognition software, help with communication. Robotics, including exoskeletons and robotic arms, assist with daily tasks. Home adaptations, like ramps and grab bars, improve accessibility.
Lifestyle Management and Support
Lifestyle management is crucial for individuals with muscular system diseases. Dietary modifications can help. Eggs, fish, chicken breast, and cottage cheese provide protein for muscle growth. Green tea contains antioxidants. Tuna offers omega-3 fatty acids. Pumpkin seeds and oats provide essential nutrients. Individuals with DMD need routine dietary assessment.
Calorie needs may change as mobility decreases. Long-term corticosteroid use requires nutritional management. This addresses weight gain and bone fragility. Adequate protein intake maintains muscle health. Limiting saturated fats and high salt reduces cardiac problems. Drinking water and eating fiber-rich foods prevent digestive issues. Calcium and vitamin D are crucial for bone health.
Muscular system diseases are diverse, with varied causes, symptoms, and impacts on individuals. These conditions range from genetic disorders to those caused by injury or infection. Early and accurate diagnosis is critically important for effective management and improving quality of life. Individuals should seek professional medical consultation for any persistent or concerning muscular symptoms. This blog serves as an informational guide, not a substitute for medical advice.

