A tortuous aorta describes your body’s largest artery when it appears abnormally twisted, curved, enlarged, or narrowed. This vital vessel carries oxygen-rich blood from your heart to your entire body.
While a tortuous shape often develops with age and is usually benign, understanding this tortuous condition is important for your overall heart health. A tortuous path for blood can sometimes matter, making this tortuous change worth knowing. A tortuous vessel warrants your attention.
Key Takeaways
A tortuous aorta means your body’s main artery has an abnormal twist or curve. This often happens as you get older.
Most tortuous aortas are not serious. They are a normal part of aging. But some conditions, like Arterial Tortuosity Syndrome, can make it more serious.
A tortuous aorta can affect blood flow. This makes your heart work harder. It can also increase the risk of other heart problems.
Doctors use special scans to find a tortuous aorta. Regular check-ups are important to watch for any changes.
You can help your heart by living a healthy lifestyle. This includes eating well, exercising, and managing blood pressure. Avoid smoking.
What is a Tortuous Aorta
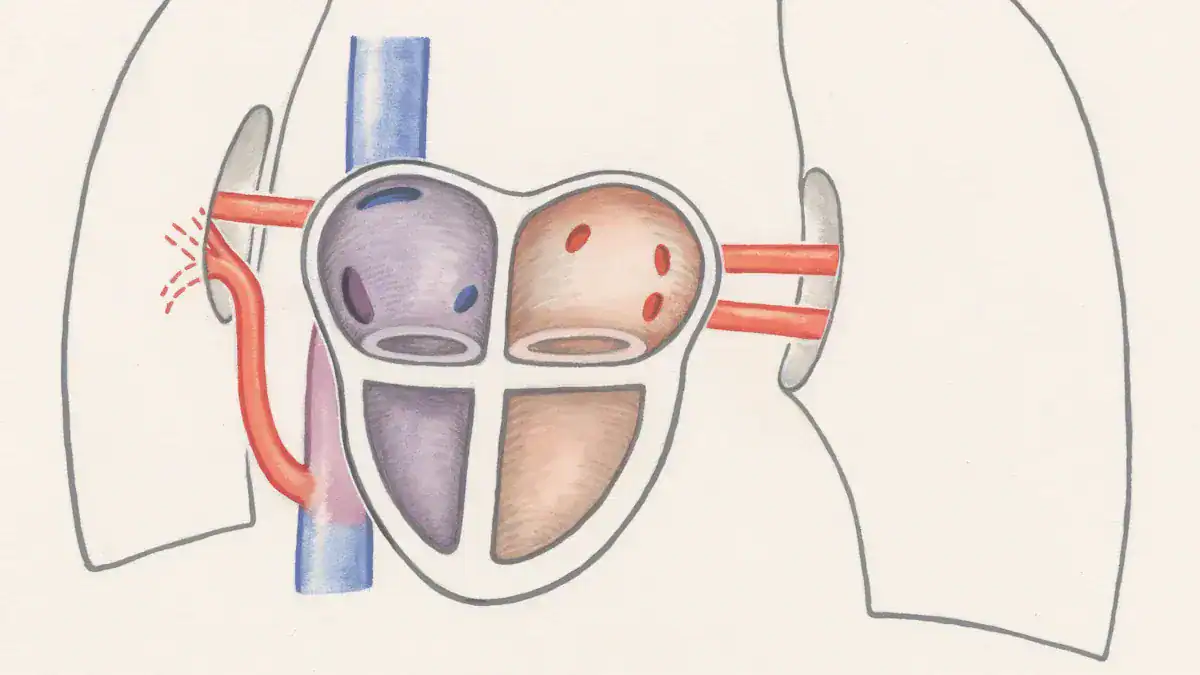
You have a complex network of blood vessels inside your body. Among them, the aorta stands out as the largest and most important artery. When doctors describe a tortuous aorta, they are talking about this major blood vessel having an abnormal shape. It might appear twisted, curved, enlarged, or even narrowed in certain places.
This change in shape is often a natural part of aging, and it is usually not a serious problem. However, understanding this tortuous condition helps you stay informed about your heart health.
Aorta’s Role in Circulation
Your heart works hard every second of every day. It pumps oxygen-rich blood to every part of your body. The aorta is the main highway for this blood. It leaves your heart, arches over, and then travels down through your chest and abdomen. From the aorta, smaller arteries branch off, carrying blood to your brain, arms, legs, and all your organs.
A healthy aorta ensures a smooth and efficient flow of blood. This smooth flow is vital for your body’s cells to get the oxygen and nutrients they need. When your aorta is healthy, your entire circulatory system benefits.
Normal vs. Tortuous Anatomy
Imagine a perfectly straight garden hose. That is similar to how a healthy, young aorta typically appears. It has a relatively smooth path. However, as you get older, your arteries can become less elastic. This can cause your aorta to become more tortuous. A tortuous aorta means it has developed more bends, curves, or twists than a straight path.
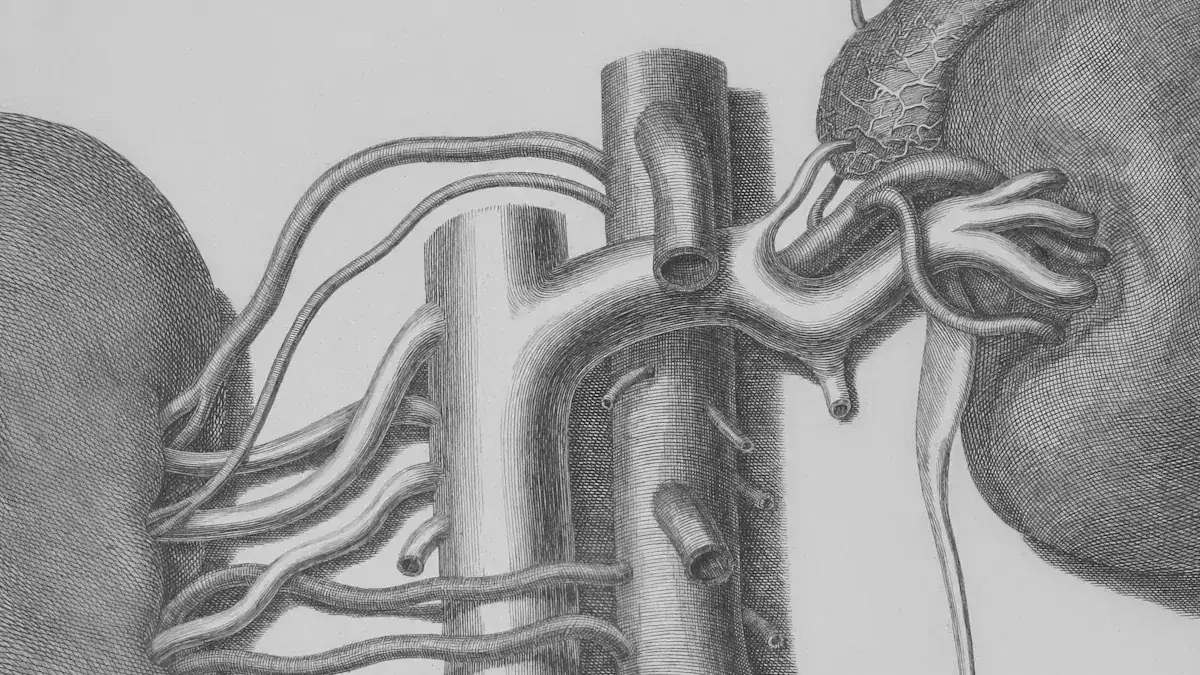
Doctors use specific measurements to define a tortuous aorta. They use a formula to quantify how tortuous your aorta is. This formula is T = (L/D – 1) * 100.
Here, ‘L’ is the actual length of a section of your aorta. ‘D’ is the straight-line distance between the start and end points of that same section. This calculation tells you the percentage of extra length your aorta has compared to a perfectly straight segment. This helps doctors understand the extent of the blood vessel tortuosity.
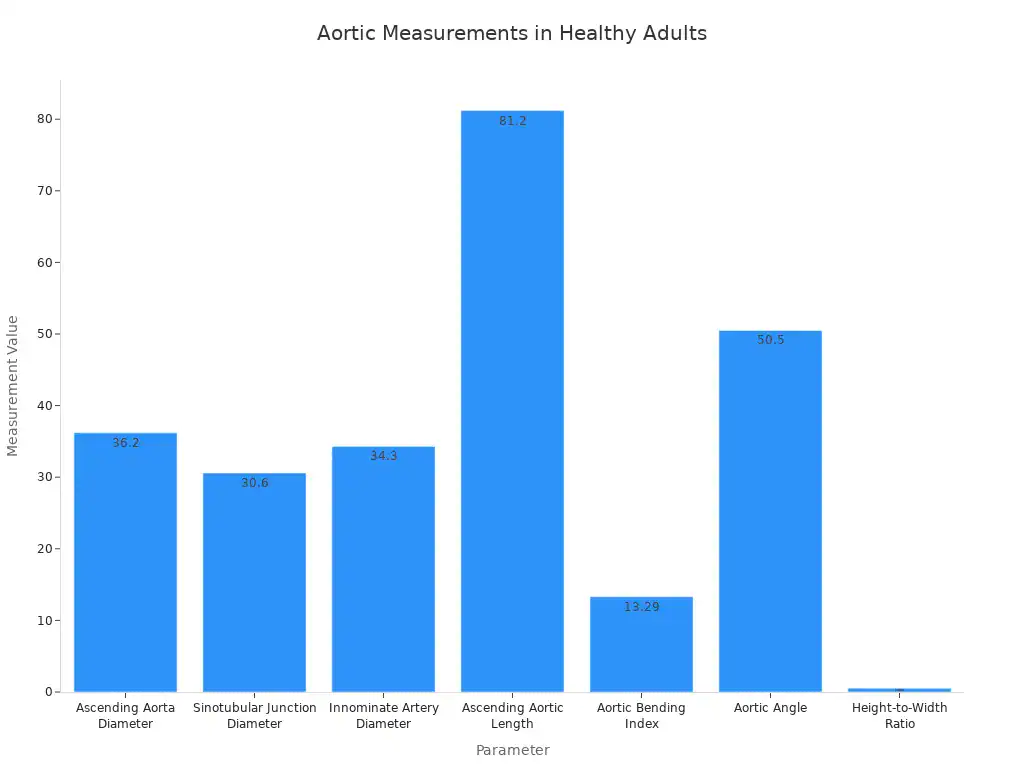
A normal aorta has specific dimensions. For example, the ascending aorta, which is the first part of the aorta leaving your heart, typically has a diameter around 36.20 mm. The length of this section, called the Ascending Aortic Length (AAL), is usually about 81.20 mm. These measurements help doctors identify when a vessel is becoming tortuous.
Parameter | Median Measurement (mm or degrees) | Q1–Q3 Range (mm or degrees) |
|---|---|---|
Ascending Aorta Diameter | 36.20 | 33.40–37.70 |
Sinotubular Junction (STJ) Diameter | 30.60 | 28.60–29.96 |
Innominate Artery Diameter | 34.30 | 31.40–36.30 |
Ascending Aortic Length (AAL) | 81.20 | 76.90–86.20 |
Aortic Bending Index (ABI) | 13.29 mm/cm | 12.71–13.78 mm/cm |
Aortic Angle | 50.5° | 47.1°–55.2° |
Height-to-Width Ratio | 0.531 | 0.47–0.60 |
This chart shows you typical measurements for a healthy adult aorta. When your aorta deviates significantly from these numbers, it might indicate a tortuous condition.
A tortuous aorta is not the only type of blood vessel abnormalities you can have. Other tortuous arteries and even tortuous veins can occur throughout your body. However, the aorta’s size and critical role make its tortuosity particularly important to monitor. A tortuous path for blood flow can sometimes create challenges for your heart. This is why doctors pay attention to any tortuous blood vessels they find.
Causes of a Tortuous Aorta
Several factors can make your aorta become tortuous. Sometimes, it is a normal part of getting older. Other times, underlying health issues or your genes play a role. Understanding these causes helps you know more about your heart health.
Age and Arterial Stiffness
Age is a major reason your aorta might become tortuous. As you get older, your arteries naturally change. They can lose some of their elasticity. This makes them stiffer. This stiffness can contribute to the development of tortuous arteries. Studies show that older individuals often have more tortuous aortas. For example, people over 65 years old show a more pronounced tortuosity in their descending thoracic aorta compared to younger individuals.
Look at this table:
Metric | < 65 Group | ≥ 65 Group | p-value |
|---|---|---|---|
Tortuosity Index | 1.05 | 1.14 | < 0.001 |
Curvature Ratio | 1.00 | 1.01 | < 0.001 |
Maximum Tortuosity | 22.24 | 27.26 | < 0.001 |
This table shows that the tortuosity index, curvature ratio, and maximum tortuosity are all higher in people aged 65 and older. This means your aorta becomes more tortuous as you age. While arterial stiffness is a factor, research suggests that age, body mass index, and diabetes are more directly linked to aortic tortuosity.
Underlying Medical Conditions
Sometimes, a tortuous aorta points to other health problems. Certain medical conditions can cause your aorta to twist or curve more than usual. These conditions include:
Marfan syndrome: This condition can make your aorta more tortuous.
Loeys-Dietz syndrome: You might see very increased tortuosity with this syndrome.
Heritable thoracic aortic disease: This can also lead to increased tortuosity in your arteries.
Hypertension (high blood pressure): High blood pressure can make your aorta longer and more tortuous.
Rare vascular disease and other connective tissue disorders can also cause blood vessel abnormalities.
These conditions can affect the structure of your tortuous blood vessels.
Genetic Factors and Disorders
Your genes can also play a part in whether you develop a tortuous aorta. Some people inherit conditions that make their arteries more prone to twisting. These genetic links include:
TGFBR1/2 mutations, linked to Loeys-Dietz syndrome.
SLC2A10 mutations, associated with arterial tortuosity syndrome.
FBN1 mutations, found in Marfan syndrome.
SMAD3 mutations, connected to aneurysms-osteoarthritis syndrome.
TGFB2 and PRKG1 mutations, implicated in familial thoracic aneurysm and aortic dissection.
FBLN4/EFEMP2 mutations, causing a rare form of cutis laxa.
ATP7A mutations, linked to Menkes disease and occipital horn syndrome.
These genetic changes can affect the connective tissues that support your arteries. This can lead to tortuous arteries and sometimes even tortuous veins in other parts of your body.
Arterial Tortuosity Syndrome: A Specific Concern
Understanding the Syndrome
Arterial Tortuosity Syndrome (ATS) is a specific and more serious condition. It is not just a simple bend in one artery. You see widespread elongation and twisting in many of your arteries. Doctors call this generalized arterial tortuosity. You also might have narrowing in some areas.
This narrowing is called focal stenosis. A key feature of arterial tortuosity syndrome is a change in your SLC2A10 gene. This genetic mutation causes the syndrome. ATS is very rare. Less than 1 in 1,000,000 people globally have it. It is an extremely rare disease.
Doctors diagnose arterial tortuosity syndrome by looking for generalized arterial tortuosity. They do this through a physical exam, an echocardiogram, or CT or MRI imaging. They also perform genetic testing for the SLC2A10 gene. In classical cases, your family history, physical exam, and imaging can strongly suggest arterial tortuosity syndrome.
Your pulmonary arteries, which carry blood to your lungs, are often prone to narrowing with ATS. This makes the condition more complex. This is a truly tortuous condition. Understanding arterial tortuosity syndrome is crucial.
ATS vs. General Tortuosity
You might wonder how arterial tortuosity syndrome differs from general tortuosity. General tortuosity often happens as you age. It usually affects your aorta or a few other large tortuous arteries. It is often a benign change. However, arterial tortuosity syndrome is different. It is a distinct and more severe condition. It involves widespread tortuous arteries throughout your body. This means many of your tortuous blood vessels are affected. It is not just an age-related change. ATS is a genetic disorder. It causes significant problems with your connective tissue. This makes your tortuous arteries much more fragile. You need to understand this difference.
General tortuosity is often harmless. Arterial tortuosity syndrome requires careful medical attention. This specific arterial tortuosity syndrome presents unique challenges. The widespread nature of this tortuous condition sets it apart. You will find many tortuous vessels. This makes it a very tortuous situation for your body.
How a Tortuous Aorta Affects Your Heart
A tortuous aorta can change how your cardiovascular system works. The twists and turns in this major blood vessel can create challenges for your heart. You need to understand these potential impacts.
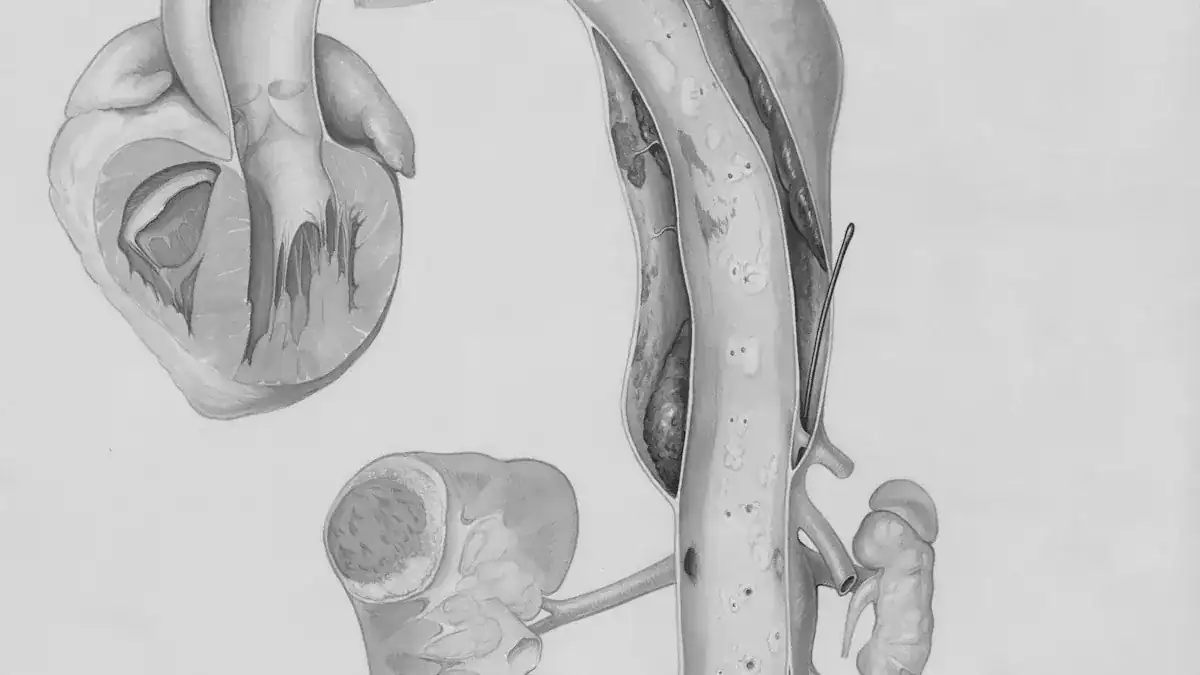
Impact on Blood Flow and Pressure
When your aorta is tortuous, it does not provide a straight path for blood. This can affect how blood moves through your body. You might experience lower blood flow velocity across all regions of your aorta. Imagine water flowing through a straight pipe versus a very winding one; the water in the winding pipe slows down.
A tortuous path also creates an asymmetrical flow profile. This means blood does not flow evenly. It can also lead to abnormal wall shear stress patterns. Wall shear stress is the force blood exerts on the vessel walls. Low wall shear stress is common in tortuous aortas. You often see this in areas with vortices and recirculation zones.
These are like little whirlpools inside your artery. However, acute angulation, a sharp bend, can create areas of high blood flow velocity. This mix of high and low stress can be hard on your tortuous blood vessels.
These altered hemodynamics, or changes in blood flow, impact your aortic wall. They can cause vessel wall remodeling. This means your artery changes its structure. This process can increase left ventricular afterload. Afterload is the pressure your heart must work against to pump blood out.
An increased afterload makes your heart work harder. These changes are linked to cardiovascular events. Aortic morphological changes, like tortuosity, alter hemodynamic processes. This increases the burden on your cardiovascular system. It also elevates your risk of cardiovascular disease.
Risk of Dilation or Aneurysm
A tortuous aorta can sometimes lead to more serious problems. The constant stress from altered blood flow and pressure can weaken your aortic wall. This weakening can cause your aorta to dilate, or widen. In some cases, it can lead to an aneurysm. An aneurysm is a bulge in your artery wall. It can be dangerous if it ruptures.
If you have arterial tortuosity syndrome, this risk becomes much higher. The widespread nature of tortuous arteries in arterial tortuosity syndrome makes them more fragile. This increases the chance of dilation or aneurysm formation. Your heart works harder to push blood through these compromised vessels. This can strain your heart over time.
Symptoms to Watch For
Many people with a tortuous aorta have no symptoms. Doctors often discover it during tests for other conditions. However, if the tortuosity is severe, or if you have arterial tortuosity syndrome, you might experience symptoms. These symptoms occur because your heart works harder or blood flow is restricted.
You might notice:
Shortness of breath, especially with activity.
Chest pain or discomfort.
Fatigue.
Swelling in your legs or ankles.
Dizziness or lightheadedness.
In severe cases, especially with arterial tortuosity syndrome, the increased workload on your heart can lead to heart failure. This is a serious condition where your heart cannot pump enough blood to meet your body’s needs. You might also face a higher risk of heart attacks or other cardiovascular complications. If you experience any of these symptoms, you should talk to your doctor. They can assess your condition and provide guidance.
Diagnosis and Management
Diagnostic Imaging
When doctors suspect you have a tortuous aorta, they use special imaging tests. Multidetector Computed Tomography (MDCT) is the most effective way to get a rapid and comprehensive evaluation. It gives doctors a detailed view of your aorta. While MRI offers good views of vascular changes, it often takes a long time. You might need prolonged sedation for an MRI.
Sonography can identify tortuous vessels in areas it can reach, but it cannot show all your blood vessels. MDCT helps overcome these limitations. Doctors are also improving CT technology to reduce concerns about radiation and contrast.
For routine follow-up of mild, asymptomatic cases, you might have yearly chest X-rays, echocardiography, Doppler sonography, or MRI. Doctors usually reserve MDCT for emergencies or when you cannot have an MRI.
Monitoring and Follow-Up
After diagnosis, monitoring your tortuous aorta is very important. Your doctor will tell you how often you need check-ups.
If you have isolated tortuous vessels without an aneurysm, you will have clinical follow-up. Doctors do not typically order specific imaging unless you develop new symptoms.
For aortic ectasia with tortuous features, you need annual imaging. This helps monitor the growth rate. A growth of 3 mm per year or more is a high-risk sign.
If your aortic dimensions are borderline, doctors suggest follow-up imaging within 6-12 months.
The European Society of Cardiology also recommends annual follow-up imaging for aortic ectasia and tortuous aortas. They also watch for a growth rate of 3 mm per year or more.
You will have more frequent imaging if you have high-risk features. These include a family history of aortic problems or connective tissue disorders. This helps manage your tortuous condition effectively.
Treatment and Lifestyle
Managing a tortuous aorta involves treating any underlying health issues and making healthy lifestyle changes.
You must avoid smoking and all tobacco products. This includes vaping and smokeless tobacco.
Eat a heart-healthy diet. Focus on foods low in saturated fat and cholesterol.
Maintain a healthy weight. Talk to your healthcare provider to find your ideal range.
Incorporate regular exercise into your daily routine. Increase your overall physical activity.
Manage your blood pressure, cholesterol, and blood sugar. Use lifestyle changes and prescribed medications.
Attend annual checkups and all other medical appointments.
A tortuous aorta is often a benign, age-related change. However, it can also be part of more serious conditions, such as arterial tortuosity syndrome. This specific arterial tortuosity syndrome involves widespread tortuous vessels. Understanding arterial tortuosity syndrome is key.
A tortuous path affects blood flow and pressure, impacting your heart. You need to monitor any tortuous changes. Imaging helps diagnose a tortuous vessel. Manage underlying conditions for your tortuous condition. A heart-healthy lifestyle supports your tortuous arteries. Regular check-ups guide you with your tortuous health. This proactive approach helps you protect your heart.