You may often find your legs hurting at night. This can disrupt your sleep. You might ask, “Why do my legs hurt at night?” This leg pain at night can stem from many different sources. This experience is quite common, affecting many people. For example, nighttime leg pain often increases as you get older. It also appears more frequently in women. Factors like education level and employment status can also link to its occurrence. These range from simple muscle fatigue to more serious health issues. Understanding the potential causes helps you find appropriate relief. Knowing the common causes of leg pain is the first step.
Key Takeaways
Leg pain at night has many causes. These include muscle cramps, restless legs syndrome, and nerve damage. Poor circulation and joint problems can also cause pain.
Your daily habits affect leg pain. Overusing muscles, not drinking enough water, and sitting too long can make legs hurt. Wearing bad shoes also plays a role.
Some medical conditions cause leg pain. Diabetes, kidney disease, and thyroid problems can lead to discomfort. Certain medicines can also cause leg cramps.
You can find relief and prevent leg pain. Stretch your legs, drink enough water, and eat healthy foods. Elevating your legs and using warm compresses can also help.
See a doctor if pain continues or worsens. Look for swelling, numbness, or skin changes. Sudden, severe pain needs immediate medical help.
Common Causes of Leg Pain at Night

Many reasons can make your legs hurt at night. These reasons range from simple muscle issues to more complex health problems. Understanding these common causes of leg pain helps you know what might be happening.
Nighttime Leg Cramps
You might experience sudden, strong muscle tightening in your legs. These are called nighttime leg cramps. They often happen in your calf muscles. These cramps can also affect your feet or thighs. Nighttime leg cramps are very common. They can wake you up from sleep. These muscle spasms can be quite painful.
Several things can trigger these nocturnal leg cramps. You might sit for long periods during the day. Overusing your muscles can also cause them. Standing or working on hard concrete floors can lead to leg cramps at night. Poor posture throughout the day also plays a role. Certain medical conditions are linked to nocturnal leg cramps. These include kidney failure, diabetic nerve damage, and issues with blood flow. Mineral deficits, like low calcium, potassium, or magnesium, can also cause them.
Here are some common triggers for leg cramps at night:
Being 50 years old or older
Overworking your muscles
Sitting too long without moving
Not drinking enough water (dehydration)
Standing too long on hard surfaces
Diabetes
Neurological conditions, such as Parkinson’s disease
Drinking too much alcohol
Low blood sugar
Hormone problems, like an underactive thyroid
Flat feet
Pregnancy
Problems with blood flow
Nerve damage
Some medications can also cause leg cramps as a side effect. These include certain drugs for asthma, heart conditions, and depression. For example, diuretics, which are “water pills,” can lead to leg cramps.
Many medical conditions are associated with leg cramps:
Associated Medical Condition |
|---|
Cancer treatment |
Cardiovascular disease |
Cirrhosis |
End-stage renal disease and hemodialysis |
Lumbar canal stenosis |
Neurologic deficit |
Osteoarthritis |
Peripheral neuropathy |
Peripheral vascular disease |
Pregnancy |
Venous insufficiency |
Restless Legs Syndrome
Restless Legs Syndrome (RLS) is a condition that causes an uncontrollable urge to move your legs. This urge often comes with uncomfortable sensations. People describe these sensations as crawling, tingling, pulling, or aching legs. These feelings usually start or get worse when you rest, especially in the evening or at night. Moving your legs, like walking or stretching, often makes the feelings go away, at least for a short time. RLS is a common cause of leg pain at night.
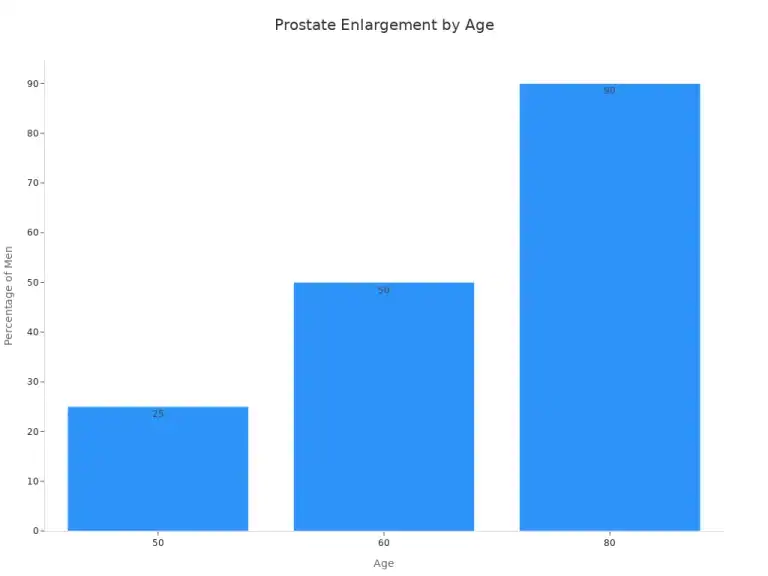
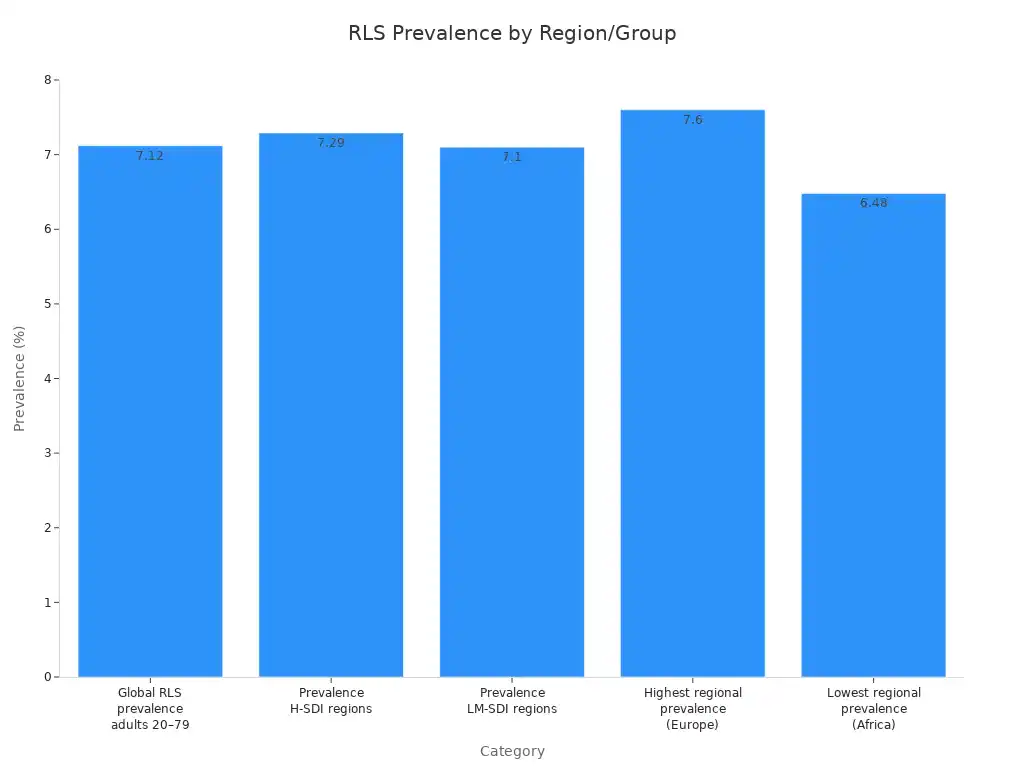
RLS affects many people worldwide. About 7.12% of adults aged 20–79 years experience RLS globally. This means around 356.07 million individuals have it. The prevalence is similar in different regions. Europe has the highest regional prevalence at 7.60%. Africa has the lowest at 6.48%.
Doctors use specific criteria to diagnose restless leg syndrome:
You feel an irresistible urge to move your legs. This urge usually comes with uncomfortable sensations.
These symptoms begin or get worse when you are resting or inactive, like sitting or lying down.
Moving your legs, such as walking or stretching, partially or totally relieves the symptoms. This relief lasts as long as you keep moving.
The symptoms are worse in the evening or at night than during the day. Sometimes, they only happen in the evening or at night.
Another medical condition or behavior does not fully explain these symptoms.
Peripheral Neuropathy
Peripheral neuropathy happens when nerves outside your brain and spinal cord get damaged. These nerves send messages between your brain and the rest of your body. When they are damaged, they cannot send messages correctly. This can cause leg pain at night. You might feel numbness, tingling, weakness, or burning pain in your legs and feet. This aching legs sensation can be constant.
Many things can cause peripheral neuropathy. Diabetes is a very common cause. High blood sugar levels can damage nerves over time. Other causes include:
Autoimmune diseases: Conditions like lupus, rheumatoid arthritis, and vasculitis.
Medications and toxins: Chemotherapy drugs, certain antibiotics, and exposure to heavy metals.
Infections: Viruses like HIV, bacteria causing Lyme disease, or shingles.
Genetic conditions: Inherited disorders that affect nerve function.
Trauma or surgery: Direct injury to nerves or swelling that presses on them.
Vascular disorders: Problems with blood flow to the nerves.
Nutritional deficiencies: Not getting enough vitamins, especially B vitamins.
Kidney failure: When your kidneys do not work well, toxins can build up and damage nerves.
Chronic alcoholism: Long-term alcohol abuse can harm nerves.
Sometimes, the causes remain unknown. Doctors call this idiopathic neuropathy.
Sciatica
Sciatica is a type of leg pain that comes from your sciatic nerve. This nerve is the longest in your body. It runs from your lower back, through your hips and buttocks, and down each leg. When something presses on or irritates this nerve, you feel sciatica. This can cause significant leg pain at night.
The pain often feels like a sharp, shooting pain. It can also feel like a burning sensation or tingling. You might feel weakness in the affected leg. Sciatica usually affects only one side of your body. A herniated disc in your spine is the most common cause. This happens when a disc between your vertebrae bulges out and presses on the nerve. Other causes include bone spurs, spinal stenosis (narrowing of the spinal canal), or a tumor. The pain can worsen when you lie down, making it hard to sleep.
Lifestyle and Activity Factors

Your daily habits and activities significantly impact how your legs feel at night. Certain lifestyle choices can directly cause or worsen leg pain. Understanding these factors helps you make changes for better comfort.
Muscle Overuse
You might experience leg pain at night because you overused your muscles during the day. Hard work or sports can lead to muscle overuse syndrome. Strenuous activities like hiking, running, or jumping excessively often cause constant leg pains. After intense exercise, you can get strained muscles. This pain typically lasts for 3 to 7 days. The peak pain often occurs on day 2. In severe cases, the pain may persist for up to a week. Muscle cramps are sudden, involuntary contractions. They often happen after exercise. Many people experience leg cramps at night. Straining or overusing a muscle is a common cause of these leg cramps. You can prevent some forms of leg pain by stretching muscles before and after physical activity. Eating foods rich in potassium, like chicken and bananas, also helps prevent muscle and tendon injuries in your legs.
Dehydration
You might hear that dehydration causes leg cramps. The dehydration and electrolyte depletion hypothesis suggests that heavy sweating without enough fluid replacement can increase fluid osmolality. This causes fluid to move, increasing pressure on nerve pathways. This pressure could lead to muscle cramps. However, scientific evidence for this link is inconsistent. Studies have found no association between electrolyte levels and hydration status with exercise-associated muscle cramping. Significant dehydration does not always affect skeletal muscle cramp frequency. Research shows that even 3% hypohydration does not impact the threshold frequency of electrically induced cramps. The dehydration and electrolyte depletion hypothesis does not offer plausible explanations for muscle cramps. Maintaining hydration by drinking at least eight glasses of water daily is still important for overall health.
Sedentary Habits
Prolonged inactivity can contribute to leg pain at night. Sitting for long periods impacts your leg circulation. This is especially true if you have conditions like Peripheral Artery Disease (PAD). Sedentary lifestyles can decrease muscle and tendon length and flexibility. This can lead to leg cramps. Poor blood circulation, a direct result of sedentary habits, contributes to leg cramps, especially at night. General immobility during sleep can further decrease circulation. A study found a strong link between nocturnal leg cramps and a sedentary lifestyle. This highlights the importance of physical activity.
Poor Footwear
Your shoes can also cause leg pain at night. Wearing poorly fitting shoes strains your foot muscles throughout the day. Narrow-toed shoes, high heels, and shoes with poor foot support can cause sore feet. They can also lead to calluses, blisters, and bunions. Uncomfortable footwear, such as heels or flats without enough stability or cushioning, can aggravate nerve and muscle issues in your feet and legs. This can result in nightly leg cramps and aching legs. Choose shoes that fit well and offer good support to prevent this type of leg pain at night.
Circulatory Issues
Problems with your blood circulation can often cause leg pain at night. Your blood vessels carry blood throughout your body. When these vessels do not work well, your legs can hurt.
Peripheral Artery Disease
Peripheral Artery Disease (PAD) happens when arteries in your legs narrow. This reduces blood flow to your limbs. You might notice leg pain that intensifies at night. This happens because lying down decreases blood circulation. The horizontal position can make blood flow restriction worse, causing heightened pain or cramping. In severe cases, you may even feel pain in your feet or toes while resting. This pain can be strong enough to stop you from sleeping.
Varicose Veins
Varicose veins are swollen, twisted veins you can see under your skin. They often appear in your legs. Inefficient blood flow leads to increased pressure in your veins. This pressure can damage vein walls and valves. Blood then collects because the valves do not work well. This causes high pressure and unpleasant feelings. Stagnant blood in varicose veins can also inflame nerves in your legs. Chronic venous insufficiency, linked to varicose veins, means your leg muscles may not get enough oxygen. This can lead to aching legs, especially when you are resting. Your body often urges you to move your legs to help blood flow through muscle compression.
Deep Vein Thrombosis
Deep Vein Thrombosis (DVT) is a serious condition. It happens when a blood clot forms in a deep vein, usually in your leg. This can cause significant leg pain at night. Several factors can increase your risk for DVT. You might have a higher risk if you are obese or over 60. An inherited tendency for blood clots also plays a role. Cancer patients, pregnant individuals, and those taking hormonal birth control face increased risk. Recent surgery or being immobilized for long periods also raises your chances. Prolonged inactivity, like long car trips or bed rest, slows blood flow. Injury to a vein, such as from a fracture or certain surgeries, can also cause DVT. Conditions that make blood clot easily, like heart disease or autoimmune disorders, are risk factors. Being overweight, smoking, or having a family history of blood clots also increases your risk.
Inflammatory and Joint Conditions
Inflammation and joint problems can also make your legs hurt at night. These conditions often cause pain that worsens when you rest.
Arthritis
Arthritis is a condition that causes joint inflammation. This can lead to significant leg pain at night. Arthritis may contribute to this discomfort through its link with Restless Legs Syndrome (RLS). RLS symptoms include uncomfortable sensations in your legs. You might feel aching, tingling, throbbing, burning, pulling, itching, crawling, or creeping. You also feel a strong urge to move your legs. These symptoms often get worse at night or when you are inactive. They can range from uncomfortable to very painful. These feelings frequently disrupt your sleep, adding to your nocturnal leg discomfort. Studies have identified arthritis as a comorbidity for leg cramps. This means arthritis often occurs with leg cramps. For example, the Roffe 2002, Hallegraeff 2012, and Oboler 1991 studies all noted arthritis as a comorbidity for nocturnal leg cramps.
Tendinitis
Tendinitis happens when a tendon becomes inflamed. Tendons are thick cords that connect your muscles to your bones. When you have tendinitis in your legs, you can feel pain, especially after activity. This can lead to aching legs. Overuse is the most common cause. This involves repetitive stress from activities like sports or work. You might also get tendinitis from sudden movements or an injury. Certain medications can cause tendinitis as a side effect. These include statins, which lower cholesterol, and fluoroquinolone antibiotics. Underlying medical conditions like diabetes, rheumatoid arthritis, or gout can also cause tendinitis. As you get older, repetitive motions can injure the tendon where it attaches to the bone. This causes inflammation.
Bursitis
Bursitis is the inflammation of a bursa. A bursa is a small, fluid-filled sac that cushions bones, tendons, and muscles near your joints. When bursitis affects your hip or knee, it can cause leg pain at night. You might feel tenderness when you press the side of your hip. Lying on that side in bed can also cause pain. Aches that wake you at night are common. The pain can interrupt your sleep more than two nights a week. The pain is often worse at night because lying directly on the inflamed bursa increases pressure. Your hip muscles can also tighten while you sleep, which can spike the pain. Hip bursitis often feels worse at night because lying down puts added pressure on your pelvic area.
Other Medical Conditions
Sometimes, other medical conditions can cause your legs to hurt at night. These conditions affect your body in ways that lead to discomfort in your legs.
Diabetes Complications
Diabetes can lead to several complications that cause leg pain at night. Diabetic neuropathy is nerve damage from high blood sugar. This condition often causes tingling, burning, discomfort, or shooting pains in your legs. These sensations are frequently worse at night. This nocturnal pain can disrupt your sleep and daily activities. Peripheral artery disease (PAD) is another diabetes complication. It typically does not cause night pain unless the condition has progressed to a very advanced stage.
Kidney Disease
Kidney disease can also cause leg pain at night. If you have chronic kidney disease (CKD), you might experience Restless Legs Syndrome (RLS). This condition causes uncomfortable sensations in your legs, like burning, aching, or prickling, making you want to move them. Nerve damage from diabetes, which often occurs with kidney disease, can also contribute to RLS and leg discomfort. Low iron levels or not enough erythropoietin, a hormone healthy kidneys produce, are common in CKD patients. This leads to anemia, which doctors believe contributes to RLS. Studies also suggest a link between low parathyroid hormone (PTH) levels, often monitored in kidney disease patients, and RLS.
Thyroid Disorders
Your thyroid gland produces hormones that control many body functions. Thyroid disorders can cause leg pain or leg cramps. Hypothyroidism, an underactive thyroid, can cause leg swelling, pain, weakness, leg cramps, fatigue, and stiffness. Many people with newly diagnosed hypothyroidism report neuromuscular complaints. These include muscle weakness, aches, and cramping. Hyperthyroidism, an overactive thyroid, can also lead to muscle weakness and, less commonly, cramping.
Nutritional Deficiencies
Not getting enough of certain nutrients can also be causes of leg pain at night. A lack of specific vitamins and minerals can lead to uncomfortable leg sensations. For example, low levels of vitamin D and iron can contribute to leg pain and motor symptoms. Iron deficiency, or its incorrect use in the brain, can cause restless legs. Folate and magnesium deficiencies may also contribute to RLS. These deficiencies can lead to uncomfortable leg sensations or aching legs.
Medication Side Effects
Some medications you take can cause leg pain or leg cramps as a side effect. Diuretics, often called “water pills,” can lead to leg cramps. They cause your body to lose electrolytes like potassium and magnesium. This imbalance can result in leg cramps. Beta-blockers, used for high blood pressure, can narrow arteries. This reduces blood flow to your limbs, causing cramping and discomfort. ACE inhibitors, also for high blood pressure, can cause potassium buildup. This leads to aching muscles, joints, and bones. Other medications, like certain antipsychotics, beta-agonists for respiratory conditions, and some antibiotics, can also cause muscle stiffening or leg cramps.
When to Seek Medical Attention
You might experience leg pain at night for many reasons. Some causes are minor, but others need a doctor’s care. You should know when to seek medical attention for your leg discomfort.
Persistent Pain
If your leg pain at night continues for several days or weeks, you should talk to a doctor. Do not ignore pain that gets worse over time. Persistent discomfort can signal an underlying issue. This might be a chronic condition or something that needs specific treatment. A doctor can help you understand why your legs hurt and find the right solution.
Swelling or Redness
You should seek medical help if you notice swelling, redness, or warmth in your leg. These signs can point to inflammation, infection, or a blood clot. A blood clot, like deep vein thrombosis, needs urgent care. It is important to get these symptoms checked quickly. A doctor can perform tests to find the exact cause and start treatment.
Numbness or Weakness
If you experience numbness, tingling, or weakness in your legs, consult a healthcare professional. These symptoms suggest nerve damage or compression. You might also feel persistent aching legs with these sensations. Nerve issues can worsen without proper care. Early diagnosis helps prevent further problems and can improve your quality of life.
Skin Changes
Look for changes in your skin. If your leg skin becomes discolored, shiny, or develops sores that do not heal, see a doctor. These changes often indicate poor circulation. They require prompt medical evaluation. For example, a bluish tint or cold skin can mean blood flow problems. Catching these signs early helps manage the condition effectively.
Sudden Severe Pain
Seek immediate medical attention for sudden, severe leg pain. This is especially true if the pain comes with other symptoms like chest pain or shortness of breath. These could be signs of a serious condition, such as a blood clot that has traveled to your lungs. Do not wait if you experience intense, abrupt pain in your leg.
Relief and Prevention Strategies
You can take many steps to find relief and prevent your legs from hurting at night. These strategies range from simple daily habits to specific treatments. Understanding these options helps you manage your discomfort effectively.
Stretching and Exercise
Regular stretching and exercise can significantly reduce leg pain. Stretching your muscles before bed helps prevent muscle spasms and leg cramps.
Standing Calf Stretch: Stand facing a wall. Place one leg forward with a bent knee. Keep the other leg back with a straight knee. Make sure both feet stay flat on the floor. Lean towards the wall. Hold this position for 10-30 seconds. Perform 2-3 stretches on each leg every night.
Standing Hamstring Stretch: Place one heel on a chair. Keep your knee straight. Hold onto something for balance. Bend at your waist, keeping your back straight. Hold for 10-30 seconds. Perform 2-3 stretches on each leg every night.
Seated Hamstring Stretch: Sit on the side of your bed. Extend one leg and keep the other foot on the floor. Bend at your waist, keeping your back straight. Hold for 10-30 seconds. Perform 2-3 stretches on each leg every night.
A 2012 study looked at 80 adults over 55. It showed that performing nightly stretches before bed greatly improved the severity and frequency of nighttime leg cramps. Regular, moderate exercise also strengthens your leg muscles. This can make them less prone to fatigue and pain.
Hydration and Nutrition
Proper hydration and a balanced diet play a crucial role in preventing leg cramps. You should drink enough water throughout the day.
While drinking enough water is important, simply drinking plain water might not prevent all leg cramps. Electrolytes are vital for muscle health. These include sodium, potassium, magnesium, and chloride. They help your muscles work correctly and aid in water absorption.
Electrolyte-enhanced water makes muscles more resistant to cramps compared to plain water.
Drinking plain water can dilute your electrolyte concentration. This might increase your chance of getting leg cramps.
Oral rehydration solutions contain electrolytes. Doctors recommend them during moderate to intense exercise, in hot conditions, or when you are sick. They help replace lost minerals.
Some research suggests that a decrease in electrolytes due to sweating or drinking too much plain water can contribute to exercise-associated muscle cramps. Participants in one study who drank a carbohydrate-electrolyte beverage could exercise much longer before cramping. This shows a clear benefit. Current recommendations for preventing and treating leg cramps often include giving fluids and/or salt. This supports the idea that dehydration and electrolyte imbalance are linked to leg cramps.
Elevating Legs
Elevating your legs can help reduce swelling and discomfort, especially if you experience aching legs or swelling.
Elevate your legs above heart level.
Keep this position for 15-30 minutes.
Repeat this 3-4 times a day.
Elevating your legs uses gravity to improve blood flow in your lower body. This helps oxygen-depleted blood return to your heart more easily. Gravity normally makes it harder for blood to flow back through your veins, which have lower pressure than arteries. This upward flow also helps drain excess fluid. This reduces swelling (edema) caused by fluid buildup or inflammation. By allowing pooled blood to drain, leg elevation can lower pressure in your leg veins. This helps with conditions like varicose veins and eases the tenderness from tired feet after standing or sitting for a long time.
Warm Compresses
Applying warm compresses can provide significant relief for aching legs and muscle spasms. Heat therapy works in several ways to ease your pain.
It increases blood circulation. This brings more nutrition and oxygen to the affected area.
It helps reduce inflammatory factors. This lessens inflammation in the painful area.
It improves cardiovascular function and relaxes your muscles.
It increases blood supply to your muscles and helps your body tissues metabolize better.
It aids in removing cell waste.
Warm compresses can also effectively reduce inflammatory factors that reach your brain. They may even help regulate how certain immune cells (macrophages) function, potentially aiding tissue repair.
Over-the-Counter Relief
For temporary relief from legs hurting at night, you can use over-the-counter (OTC) medications. These can help manage pain and inflammation.
Ibuprofen (Advil, Motrin IB)
Acetaminophen (Tylenol)
Naproxen sodium (Aleve)
Aspirin
Always follow the dosage instructions on the package. If your pain continues or worsens, you should talk to a doctor.
Lifestyle Adjustments
Making certain lifestyle changes can greatly help in the prevention of nocturnal leg cramps and other leg pain.
Reduce caffeine intake: This is especially helpful if you have Restless Legs Syndrome.
Use heating pads or massage your legs: These techniques can help manage RLS symptoms and ease muscle tension.
Stay hydrated: This is crucial for preventing leg cramps.
Eat a balanced diet: Make sure your diet is rich in potassium and magnesium. This helps prevent future leg cramps.
Stop smoking: This is a key change if you have Peripheral Artery Disease.
Exercise regularly: Regular physical activity is good for PAD and helps prevent general muscle strain.
Maintain a healthy diet: This is recommended for PAD and helps correct vitamin deficiencies.
Correct vitamin deficiencies: You can do this through diet or supplements. Foods like leafy greens, fortified cereals, and fish are good sources.
Rest, stretch, and apply heat or ice: These are effective for relieving muscle strain.
Warm up properly, stretch, and pace yourself during physical activities: This helps prevent further muscle strain.
These adjustments can lead to long-term prevention and better sleep quality.
You now understand the many reasons for legs hurting at night. From simple muscle fatigue to serious conditions, leg pain at night has diverse origins. While many are benign, some require medical care. Listen to your body. Seek professional advice for persistent or severe nighttime leg pain. Understanding these causes helps you find relief and sleep better.
FAQ
What causes nighttime leg cramps?
Nighttime leg cramps often happen because of muscle overuse or dehydration. You might also experience them from sitting too long or standing on hard surfaces. Certain medical conditions, like diabetes or kidney issues, can also cause them. Low levels of minerals such as potassium or magnesium can also play a role.
What is Restless Legs Syndrome?
Restless Legs Syndrome (RLS) gives you an urge to move your legs. This feeling often comes with uncomfortable sensations like tingling or aching. Symptoms usually start or get worse when you rest, especially at night. Moving your legs often brings temporary relief.
What should you do for leg pain at night?
You can try stretching your legs before bed. Stay hydrated by drinking enough water throughout the day. Elevate your legs to reduce swelling. Applying warm compresses can also help. For temporary relief, you can use over-the-counter pain relievers.
What are signs you need to see a doctor for leg pain?
You should see a doctor if your leg pain is persistent or gets worse. Look for swelling, redness, or warmth in your leg. Numbness, tingling, or weakness also needs medical attention. If you notice skin changes or have sudden, severe pain, seek help right away.