
Navigating your diet can be confusing when you’re dealing with diverticular disease. Diverticulosis means you have small pouches in your colon. This condition is quite common; for example, over half of people older than 60 experience it.
For those over 70, two-thirds have it. About 10% of people younger than 40 also have diverticulosis. When these pouches become inflamed, it is called Diverticulitis. Your dietary needs change greatly depending on whether you have a flare-up or are managing the condition long-term. This food chart provides clear, actionable guidance for both scenarios.
Key Takeaways
Diverticulosis means you have small pouches in your colon. Diverticulitis is when these pouches get infected or inflamed.
During a diverticulitis flare-up, eat a low-fiber diet. This helps your colon rest and heal. Avoid high-fiber foods, red meat, and fried foods.
For long-term diverticulosis, eat a high-fiber diet. This helps prevent future flare-ups. Slowly add foods like whole grains, fruits, and vegetables.
Drink at least 64 ounces of water every day. Water helps soften your stool. This makes it easier to pass and reduces pressure in your colon.
You can eat nuts, seeds, and popcorn. Studies show these foods do not cause diverticulitis. They may even help protect you.
Diverticulosis and Diverticulitis Explained
What is Diverticulosis
Diverticulosis means you have small, bulging pouches, called diverticula, in your digestive tract. These pouches often form in your large intestine, also known as your colon.
You get these pouches when weak spots in your intestinal wall give way. Pressure inside your colon pushes through these weak spots. This creates the small, marble-sized sacs. Aging can cause these pouches. Your colonic smooth muscle may not work as well due to nerve changes. This can lead to autonomic dysregulation.
Genetic factors also play a role. Genes like ANO1 and COL6A1 affect your colon’s muscle function and tissue properties. This makes you more likely to form diverticula. Most people with diverticulosis do not have symptoms. However, some people experience mild symptoms. These symptoms include bloating, constipation or diarrhea, and cramping or pain in your lower abdomen. About 10% of people with diverticulosis may also see fresh blood in their stool due to diverticular bleeding.
What is Diverticulitis
Diverticulitis happens when these pouches become inflamed or infected. This is a more serious condition than diverticulosis. While diverticulosis is a structural issue, diverticulitis involves inflammation and infection around the pouches. You will likely experience clear symptoms during a flare-up.
These symptoms often include acute, constant abdominal pain, usually in your lower left side. You might also have fever, nausea, and vomiting. Other symptoms can include changes in bowel habits, like constipation or diarrhea, and tenderness in your abdomen. Your body shows more inflammation during diverticulitis. Blood tests can show higher levels of inflammatory markers.
Why Diet is Crucial
Your diet plays a very important role in managing both diverticulosis and diverticulitis. The right nutrition can help prevent flare-ups and manage symptoms. For example, a higher intake of dietary fiber can reduce your risk of diverticulitis. Fruit and cereal fiber are especially helpful.
Fiber helps your colon move waste better. It also affects pressure inside your colon and has anti-inflammatory effects. This is why understanding your diet is key to your digestive health.
Diet Therapy for Diverticulitis Flare-Ups
When you experience a diverticular flare-up, your diet becomes a critical part of your recovery. The goal of diet therapy for diverticulitis during this acute phase is to rest your digestive system. You reduce inflammation and allow your colon to heal. This means you temporarily switch to a very different eating plan.
Initial Clear Liquid Diet
You typically start your diverticulitis diet with a clear liquid diet. This gives your colon a complete break. You consume only liquids that you can see through. These include water, clear broths, pulp-free juices like apple or white grape, gelatin, and ice pops. You should avoid red or purple liquids, as they can be mistaken for blood in your stool.
A clear liquid diet is usually recommended for only a few days. It does not provide enough nutrients for long-term use. Healthcare providers rarely recommend it for more than five days. If you need it for a longer period, your doctor will modify it with supplements to prevent malnutrition.
Acute Diverticulitis Diet Phases
As your symptoms improve, you will gradually introduce foods to eat with diverticulitis. You move from clear liquids to a low fiber diet. This approach helps reduce pain. You can slowly add bland, starchy, and easy-to-digest foods. Think of items like those in the BRAT diet: bananas, rice, applesauce, and toast made with white bread.
Your daily fiber intake should be low during this phase. Aim for about 8 to 12 grams of fiber. The exact amount depends on how severe your diverticulitis is. You can then add other low-fiber options. These include potatoes without skin, soft proteins like eggs, chicken, turkey, or fish, and canned fruits without skins. Dairy products, if tolerated, are also an option.
Here are some examples of foods to eat with diverticulitis during this recovery phase:
Proteins: Eggs, skinless chicken or turkey, fish.
Grains: White bread, white rice, white pasta.
Fruits: Applesauce, bananas, canned peaches or pears (without skin).
Vegetables: Cooked or mashed vegetables without skins or stems, such as well-cooked carrots or potatoes (peeled).
You should eat small, frequent meals, perhaps 5-6 times a day. Each meal can include 1-2 ounces of protein. Drink plenty of water throughout the day to stay hydrated. This helps your digestion. This approach provides a sample low fiber meal plan for your recovery.
Foods to Avoid During Flares
During a diverticular flare-up, certain foods to avoid can irritate your colon and worsen your symptoms. You need to understand what not to eat. High-fiber foods are generally the first foods to limit. They can cause painful contractions in your colon.
Here is a list of common irritants and foods to avoid during a flare:
Whole Grains: These include whole wheat bread, brown rice, quinoa, and oats. Their high fiber content can be too much for an inflamed colon.
Red Meat: Some studies link red meat to inflammatory chemicals, which can worsen inflammation.
Cereals and Refined Carbohydrates: Many of these are high in sugar. They can cause gut inflammation and imbalance your gut bacteria.
Dairy Products: Many people with diverticulitis have lactose intolerance. Dairy can lead to discomfort and inflammation. High-fat dairy is also hard to digest.
Fried Foods: These are often saturated in fatty oils. They can increase gas, bloating, and inflammation.
Legumes: Beans and lentils are high in fiber. They can cause discomfort.
Spicy Foods: These are known to cause abdominal discomfort for many people.
Cruciferous Vegetables: Cabbage, broccoli, and Brussels sprouts can cause gas and bloating.
Onions and Garlic: These can also be difficult to digest for some people during a flare.
You should also avoid seeds and nuts during a flare-up. While the myth about them causing diverticulitis is largely debunked for long-term management, they can be irritating during an acute phase.
Recovery and Prevention Diet

Transitioning to High Fiber
After a flare-up, you will gradually increase fiber. This is a crucial step. You prevent gastrointestinal upset like gas and bloating. You also prevent discomfort. Slowly reintroduce solid foods. Increase your fiber intake over several days to a week or two. This helps avoid digestive upset. This approach supports overall gut health. It aids in proper stool formation and elimination. It prevents constipation and dehydration. You must gradually increase fiber to prevent digestive upset. Drink plenty of water with your increased intake.
Hydration’s Importance
Hydration is key for your colon health. Adults managing diverticular disease should aim to drink at least 64 ounces of water daily. This intake is especially important when you increase fiber consumption. Insufficient water intake with your diet can lead to constipation. Adequate fluid intake softens stool. It makes stool easier to pass through your colon. Easier stool passage reduces pressure within your colon. This is crucial for preventing complications. Proper hydration prevents constipation. Constipation is a primary trigger.
A well-hydrated body helps your colon absorb water from food. This results in soft and bulky stool. This reduces pressure on existing diverticula. Combined with fiber, it makes stool bulkier and easier to pass. This promotes smooth digestive system function. You must stay hydrated.
Nuts, Seeds, and Popcorn Myths
For a long time, medical advice for individuals with diverticular disease included avoiding certain foods. These were small, hard, or sharp items like nuts and seeds. The concern was that these food particles could get stuck in the diverticula. This could lead to inflammation and subsequent complications. However, current science challenges this belief. A large study looked at men without known diverticular disease. It found that eating nuts, corn, and popcorn did not increase the risk of incident diverticulitis. In fact, consuming nuts and popcorn may even protect you.
Here is what the study found:
Food Item | Association with Diverticulitis Risk | Hazard Ratio (95% CI) | P for Trend |
|---|---|---|---|
Nuts | Inverse (lower risk with higher intake) | 0.80 (0.63-1.01) | 0.04 |
Popcorn | Inverse (lower risk with higher intake) | 0.72 (0.56-0.92) | 0.007 |
Corn | No association | N/A | N/A |
Note: Highest intake is at least twice per week. Lowest intake is less than once per month.
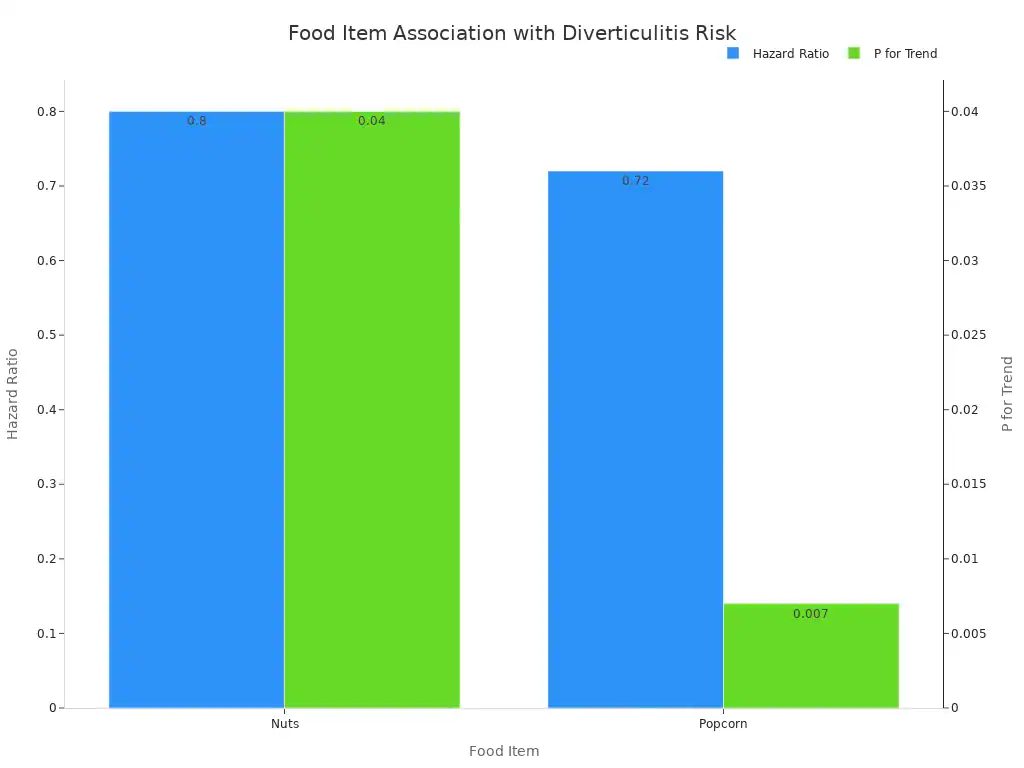
The Strate trial observed over 47,000 men for 18 years. It concluded that eating nuts and popcorn was not linked to a higher risk. Instead, a protective effect was seen.
Men who ate nuts and popcorn at least twice a week had lower hazard ratios. This was compared to those with minimal intake. No link was found between corn consumption. So, you do not need to avoid these foods. They can be part of your diverticulitis diet. They are good fiber foods. You can enjoy high-fiber foods like these. They are fiber-rich foods. These are foods to prevent diverticulitis. This diet helps you.
Here’s the Diverticulosis and Diverticulitis food chart, based on current gastroenterology and dietetic guidelines (such as those from the American Gastroenterological Association and Mayo Clinic
| Stage / Goal | Foods to Eat (Recommended) | Foods to Avoid / Limit | Notes |
|---|---|---|---|
| 1️⃣ Diverticulosis (Maintenance / Prevention Stage) | High-Fiber Diet• Whole grains (oats, brown rice, whole wheat bread, bran)• Fruits (apples, pears, berries, prunes)• Vegetables (broccoli, carrots, spinach, sweet potatoes)• Legumes (lentils, chickpeas, black beans)• Nuts and seeds (chia, flax, almonds — now considered safe) | • Processed foods (white bread, pastries, chips)• Red and processed meats• High-fat dairy• Sugary drinks and sweets | High fiber helps prevent new diverticula and reduces pressure in the colon. Aim for 25–35g fiber/day. Increase gradually and drink plenty of water. |
| 2️⃣ Mild Diverticulitis (During Flare-Up — Acute Phase) | Low-Fiber / Clear Liquid Diet (short-term)• Broth, clear soups• Gelatin, popsicles (no seeds)• Clear juices (apple, grape — no pulp)• Tea, waterOnce pain subsides → soft, low-fiber foods like:• White rice, plain pasta, eggs, canned fruit, cooked carrots | • Raw vegetables• Whole grains• Beans, lentils• Nuts, seeds, corn, popcorn• Tough meats, spicy or fried foods | A low-fiber diet allows the bowel to rest. Usually lasts 2–3 days during acute inflammation. Reintroduce fiber gradually as symptoms improve. |
| 3️⃣ Recovery / Post-Diverticulitis Phase | Transition Diet• Soft cooked vegetables• Peeled fruits (bananas, melons)• White rice, mashed potatoes, oatmeal• Lean protein (chicken, fish, eggs)Then slowly reintroduce:• Whole grains• Raw fruits & veggies• Legumes | • Fatty, fried, or spicy foods• Red meat (limit)• Alcohol, caffeine (limit if triggers) | Gradually return to high-fiber foods to restore bowel regularity. Maintain hydration and exercise. |
Diet Therapy for Diverticulosis
You manage diverticulosis long-term with specific diet strategies. These strategies aim to prevent future flare-ups of diverticulitis. Your focus shifts from resting your gut to strengthening it. This section guides you through the best practices for a diverticulosis diet.
Managing Diverticulosis Long-Term
You manage diverticulosis long-term by adopting a proactive approach. This involves consistent healthy eating habits. A high fiber diet is often recommended.
It helps maintain regular bowel movements. This reduces pressure in your colon. However, scientific findings on fiber’s effectiveness for preventing diverticulitis recurrence show some inconsistency.
Some studies indicate positive results. Others find no clear benefit. Systematic reviews also conclude that a high-fiber diet is not always consistently recommended for preventing recurrence.
Despite these varied findings, many guidelines still suggest a high-fiber approach. You should also know that the old advice about avoiding seeds, popcorn, and nuts lacks strong evidence. Studies have not shown these items increase your risk of diverticulitis or its return.
High-Fiber Food Choices
You need to choose fiber foods wisely. A sample high fiber meal plan includes a variety of plant-based options. These fiber-rich foods help keep your digestive system running smoothly. They are also foods to prevent diverticulitis.
Consider these excellent sources of fiber:
Whole Grains: You can include quinoa, bulgur, teff, and barley. Popcorn is also a good choice. Oats, shredded wheat, or bran cereals provide ample fiber. Choose whole grain breads over white varieties.
Legumes: Beans, lentils, and peas are packed with fiber. You can add them to soups, salads, or stews.
Fruits: Eat fruits with their skins on. Apples, pears, berries, and plums are great options.
Vegetables: Include a wide range of vegetables. Broccoli, carrots, spinach, and sweet potatoes are good choices.
You should gradually increase your fiber intake. This helps your body adjust. It prevents gas and bloating. Aim for 25 to 30 grams of fiber daily.
Lifestyle for Gut Health
Your lifestyle choices significantly impact your gut health. Beyond diet, other factors play a crucial role in managing diverticulosis.
Regular Physical Activity: You can reduce your risk of diverticulitis and diverticular bleeding with regular exercise. Vigorous activities like running are particularly effective. Sedentary behaviors, not just lack of recreational activity, link to an increased risk of uncomplicated diverticulosis. Obese and inactive men face a higher risk of diverticular complications. Exercise helps your gut in several ways:
It stimulates defecation. The up-and-down motion of jogging or running can help.
It decreases pressure inside your colon. This might happen by changing intestinal nerve activity or transit time.
It prevents bacteria from sitting too long in your gut. This is due to faster colon transit time.
It affects hormones that influence gut movement and secretions.
It protects against chronic blood vessel changes. These changes associate with diverticular bleeding.
It modulates your intestinal immune function and inflammation.
Probiotics: These beneficial bacteria can support your gut health. Probiotics interact with various gut cells. They regulate your immune system. They help restore a healthy gut environment. They reduce harmful bacteria. Probiotics also decrease inflammation. They improve your gut’s defense mechanisms. Specific strains, like L. acidophilus and L. salivarius Ls33, show anti-inflammatory properties. They increase beneficial compounds and decrease inflammatory ones. Dysbiosis, an imbalance of gut bacteria, links to inflammation. This creates a cycle that can lead to diverticulosis and symptoms. Probiotics may help modify this inflammation between diverticulitis episodes.
However, more research is needed to confirm their effectiveness for symptom management. There are no established protocols for probiotic use in this condition yet.



