
A low white blood cell count, also known as leukopenia, means the body has fewer white blood cells (WBCs) than normal. These WBCs are crucial for fighting infections. A healthy WBC count is vital. Doctors define leukopenia as a total WBC count below 4000/mcL. Neutropenia refers to a neutrophil count below 1500/mcL. These WBC levels have specific definitions:
Condition | Definition |
|---|---|
Leukopenia | A reduction in total WBCs to <4000/mcL. |
Neutropenia | A reduction in neutrophils to <1500/mcL. |
Severe Neutropenia | Neutrophil count <500/mcL. |
Agranulocytosis | Neutrophil count <100/mcL. |
This low WBC condition is not uncommon. About 1% of people may experience neutropenia, a specific type of low WBC. In some hospital settings, leukopenia affects over 1% of inpatients. A low white blood cell count can signal various underlying health problems, ranging from minor to serious. This blog post explores common low white blood cell count causes, helping individuals understand when to seek medical advice about their white blood cell count.
Key Takeaways
A low white blood cell count means your body has fewer cells to fight sickness. This can make you get sick more often.
Many things can cause a low white blood cell count. These include infections, certain medicines, and problems with your bone marrow.
Infections like viruses or bacteria can make your white blood cells drop. Your body uses them up quickly to fight the sickness.
Some medicines, like those for cancer or to calm your immune system, can lower your white blood cell count. This is often a side effect.
Your bone marrow makes white blood cells. Problems with your bone marrow, like certain diseases or cancers, can stop it from making enough.
Understanding Low White Blood Cell Count Causes
A low white blood cell count indicates a problem. Many different factors can lead to this condition. Understanding these factors helps identify the root cause. This section explores the main categories of low white blood cell count causes.
Infections
Infections are a common reason for a low white blood cell count. They often cause a decrease in granulocytes, a type of white blood cell. Infections are responsible for most cases of neutropenia. The body’s response to an infection can reduce the white blood cell count in two main ways.
First, infections can decrease the production of new white blood cells. Second, they can increase how quickly the body uses or destroys existing white blood cells. Sometimes, both mechanisms happen at once. For example, severe infections can overwhelm the bone marrow’s ability to produce enough wbc. The body also uses up wbc rapidly to fight the invading pathogens. This rapid use can lead to a temporary but significant drop in the overall wbc count.
Medications
Certain medications can also lower the white blood cell count. These drugs interfere with the body’s ability to make wbc. Some medications directly damage the cells that produce wbc in the bone marrow. Other drugs can suppress the immune system, which then reduces wbc production. For instance, cancer treatments like chemotherapy are well-known for causing a low wbc count. They target rapidly dividing cells, including those in the bone marrow that make wbc. Immunosuppressants, used to prevent organ rejection or treat autoimmune diseases, also reduce wbc levels.
Some antibiotics and other common drugs can also have this side effect. Doctors monitor patients closely for a low white blood cell count when they take these medications.
Bone Marrow Problems
The bone marrow is the factory for all blood cells, including wbc. Problems within the bone marrow directly lead to a reduced white blood cell count. If the bone marrow does not work correctly, it cannot produce enough wbc. This failure results in a low wbc count. Conditions like aplastic anemia cause the bone marrow to stop making enough new blood cells.
This includes red blood cells, white blood cells, and platelets. Cancers that start in the bone marrow, such as leukemia, also disrupt normal wbc production. These cancers produce abnormal wbc that do not function correctly and crowd out healthy wbc. Exposure to certain toxins, like radiation or some chemicals, can also damage the bone marrow. This damage prevents it from making enough healthy wbc.
Infections Affecting White Blood Cells
Infections are a major cause of a decreased white blood cell count. The body’s immune system uses white blood cells (wbc) to fight off invaders. Sometimes, the infection itself can reduce the number of these crucial cells. This reduction can happen in several ways. The infection might directly destroy wbc. It might also prevent the bone marrow from making enough new wbc.
Viral Infections
Many viruses can lead to a low white blood cell count. Some viruses directly attack and destroy wbc. Other viruses can suppress the bone marrow, which is where the body makes new blood cells. This suppression reduces the production of wbc.
HIV (Human Immunodeficiency Virus): This virus directly targets and destroys specific types of wbc called CD4+ T cells. This significantly weakens the immune system.
Severe Viral Infections: Viruses like influenza, measles, and Epstein-Barr virus can cause a temporary drop in the white blood cell count. The body uses up wbc quickly to fight these infections. The bone marrow may also slow down wbc production during the acute phase of the illness.
Hepatitis A and Hepatitis B: These liver infections can also lead to a temporary decrease in wbc. The body’s response to these viruses can affect bone marrow function or increase the destruction of circulating wbc.
Bacterial Infections
Severe bacterial infections can also deplete white blood cells, leading to a low white blood cell count. The body sends many wbc, especially neutrophils, to the site of infection. These cells work to kill the bacteria. When the infection is severe, the body uses up wbc faster than the bone marrow can produce them.
Rapid Depletion: In the early stages of a severe bacterial infection, the white blood cell count can drop significantly. Doctors have observed that wbc counts can fall below 3,000/μl within 10 hours of infection onset in some cases.
Overwhelmed Supply: The consumption of neutrophils at the infection site often exceeds the bone marrow’s ability to supply them. This imbalance causes the overall wbc count to decrease.
Later Drops: Sometimes, the wbc count may decrease again later in the infection. For example, in patients with severe kidney infections (pyelonephritis) and sepsis, wbc counts remarkably decreased around 72 hours after the infection started. This indicates ongoing challenges for the body to maintain adequate wbc levels. Even if a patient does not show a very high white blood cell count during a severe bacterial infection, it does not mean their wbc are not being consumed. The body might be managing the bacteria with existing circulating neutrophils, or neutrophils might not be able to reach the infected areas. However, the initial drop in wbc is mainly due to the body using more wbc than it can make. This can result in neutropenia.
Other Infections
Other types of infections can also cause a low wbc count. These include parasitic infections.
Parasitic Infections: Parasites can trigger immune responses that affect wbc levels. Some parasites can cause leukopenia, which is a general term for a low wbc count.
Plasmodium: This parasite causes malaria. Malaria can lead to a decrease in wbc.
Schistosoma: These parasites cause schistosomiasis. This condition can also affect the white blood cell count.
Leishmania: These parasites cause leishmaniasis. This infection can also result in a low wbc count.
These infections show how various pathogens can disrupt the body’s ability to maintain a healthy white blood cell count.
Medications and Treatments Impacting White Blood Cells
Medical treatments can also cause a low white blood cell count. These interventions affect the body’s ability to make wbc. Some treatments directly harm the cells that produce wbc in the bone marrow. Other treatments suppress the immune system. This then reduces wbc production.
Cancer Therapies
Cancer treatments are a major cause of a decreased white blood cell count. Chemotherapy and radiation therapy are primary examples. Chemotherapy drugs target fast-growing cells. This includes cancer cells. It also includes healthy cells in the bone marrow.
These healthy cells make wbc. When chemotherapy damages these cells, the body cannot make enough wbc. This leads to a low white blood cell count. Radiation therapy also harms bone marrow cells. This happens when radiation targets areas of the body where bone marrow is present. Both treatments reduce the body’s ability to produce new wbc.
Immunosuppressants
Doctors prescribe immunosuppressants to lower the body’s immune response. People take these drugs after organ transplants. They also take them for autoimmune diseases. These drugs work by reducing the activity of immune cells. This includes wbc. Many immunosuppressants can cause a low white blood cell count.
Some common immunosuppressants affect wbc levels:
Azathioprine (AZA) can reduce bone marrow function. This leads to lymphopenia. Lymphopenia is a sign the medicine is working.
Mycophenolate mofetil (MMF) lowers the growth of B- and T-cells. This often causes leukopenia.
Cyclophosphamide (CYC) sometimes aims for a specific low wbc count. This shows a lowered count is an expected effect.
Glucocorticoids (GC) can cause a temporary drop in lymphocytes. This happens because lymphocytes move out of the bloodstream.
Research shows a clear link between these drugs and leukopenia.
Immunosuppressive Therapy | Risk Ratio (RR) for Leukopenia | 95% Confidence Interval (CI) | P-value |
|---|---|---|---|
All Immunosuppressive Therapies vs. Placebo | 12.91 | 5.28–31.57 | < 0.05 |
AZA/6-MP vs. Placebo | 13.81 | 5.42–35.18 | < 0.05 |
MTX vs. Placebo | 3.68 | 0.16–87.14 | Not statistically significant |
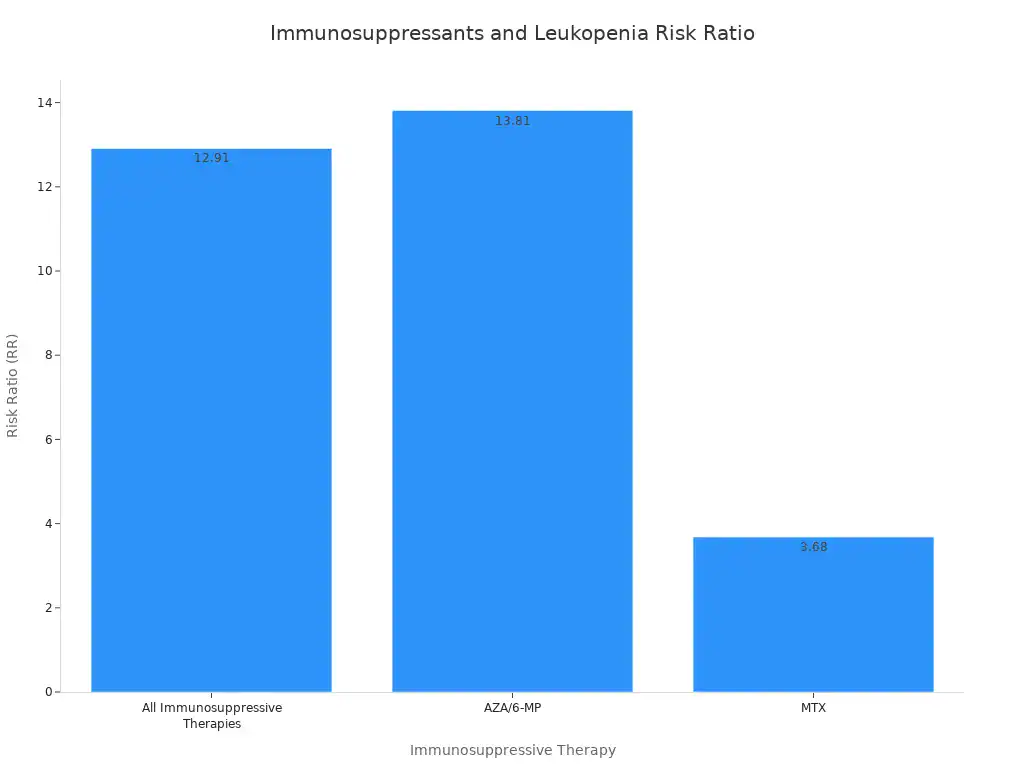
The chart above illustrates the risk. AZA/6-MP has the highest risk ratio for leukopenia. This means people taking it are much more likely to develop a low white blood cell count. This effect is often a desired outcome. It helps prevent the immune system from attacking the body. However, it also increases the risk of infection. This is because the body has fewer wbc to fight germs. This can lead to neutropenia.
Other Drugs
Many other drugs can also cause a low wbc. These are not cancer drugs or main immunosuppressants. They can still affect wbc production or survival.
Some examples of these drugs include:
Quinidine
Cephalosporin
Aminopyrine
Heavy metals
Phenothiazine
Sulfonamides
Penicillins
Interferons
Bupropion
Steroids
Antipsychotic medications (e.g., clozapine)
Other drug classes also carry this risk. These include:
Antihistamines
Antihypertensives
Antipsychotics
Anti-epilepsy drugs
Steroids
These medications can interfere with bone marrow function. They might also cause the body to destroy wbc. Doctors monitor patients taking these drugs. They check for any signs of a low wbc.
Bone Marrow Issues and Low White Blood Cells
The bone marrow acts as the body’s factory for all blood cells. This includes white blood cells (wbc). Problems within the bone marrow directly lead to a reduced white blood cell count. If the bone marrow does not work correctly, it cannot produce enough wbc. This failure results in a low white blood cell count.
Bone Marrow Disorders
Certain conditions directly affect the bone marrow’s ability to produce blood cells. Aplastic anemia is one such serious blood disorder. In this condition, bone marrow problems lead to low levels of white blood cells. These cells are essential for fighting infection and disease. Aplastic anemia typically occurs when the immune system attacks bone marrow. This attack prevents the bone marrow from producing stem cells. This then leads to low levels of white blood cells.
Doctors identify aplastic anemia through several methods. These include physical examinations and blood tests. Blood tests often include a complete blood count (CBC) with differential. This measures all five types of white blood cells. Doctors also use a peripheral blood smear to examine blood cells and platelets. A reticulocyte count checks for immature red blood cells. Genetic tests can also help. Finally, a bone marrow aspiration and biopsy obtains and examines bone marrow tissue.
Cancers of the Bone Marrow
Cancers that start in the bone marrow also disrupt normal wbc production. Leukemia is a type of cancer that affects blood-forming tissues. Leukemia cells multiply rapidly in the bone marrow. They crowd out the space and support needed for normal blood cells. This includes white blood cells. These healthy cells cannot mature and multiply properly. This leads to fewer healthy white blood cells being produced. These cells are then not released into the blood. This impairs the body’s ability to fight infections.
In a healthy person, immature stem cells in the bone marrow become either lymphoid or myeloid stem cells. Lymphoid stem cells develop into white blood cells called lymphocytes. These are part of the immune system. Myeloid stem cells develop into other white blood cells, red blood cells, and platelets. Leukemia happens when a bone marrow stem cell’s DNA changes. It becomes cancerous and multiplies quickly. This crowds out healthy cells in the blood and bone marrow. This prevents the proper development and function of healthy white blood cells.
Leukemia has different types:
Myelogenous (myeloid) leukemia: This develops from myeloid cells. Normal myeloid cells typically become red blood cells, white blood cells, and platelets.
Lymphocytic leukemia: This develops from lymphoid cells. Normal lymphoid cells are crucial for the body’s immune system. They develop into white blood cells like lymphocytes.
Doctors also classify leukemia by how fast it grows:
Acute leukemia: This impacts immature cells. It prevents their development and function. These cells multiply rapidly. This leads to aggressive disease progression.
Chronic leukemia: This involves mature or partially mature cells. They multiply more slowly. They are less aggressive than acute leukemia.
Multiple myeloma is another cancer affecting the bone marrow. It involves plasma cells, a type of wbc. These abnormal plasma cells build up in the bone marrow. They can crowd out healthy blood cells. This leads to a low white blood cell count and other blood problems. This can also result in neutropenia.
Environmental Factors
Exposure to certain environmental toxins can also damage the bone marrow. This damage prevents it from making enough healthy wbc. Cadmium, a heavy metal, is one such environmental hazard. Studies show it impairs bone marrow hematopoietic cells. Chronic exposure to cadmium chloride in Japanese quails damaged these cells. It also caused severe red blood cell damage and liver problems.
A study of US adults found many environmental chemicals linked to immune system markers. These chemicals included metals and smoking-related compounds. Researchers found 33 chemicals associated with white blood cell counts. These were among 71 environmental chemicals linked to at least one immune measure. These findings show how environmental factors can contribute to a low wbc. This can lead to a low white blood cell count.
Autoimmune and Other Conditions
Systemic diseases and other factors can also contribute to a low white blood cell count. These conditions often involve the body’s immune system or its ability to get enough nutrients. They can lead to problems with white blood cell production or survival.
Autoimmune Diseases
Autoimmune diseases occur when the body’s immune system mistakenly attacks its own healthy tissues. This attack can lead to a low white blood cell count. The immune system targets and destroys white blood cells (wbc) or the cells that make them. This results in a low wbc.
Systemic Lupus Erythematosus (SLE), often called lupus, is a common autoimmune disease. Up to 50% of people with SLE have reduced white blood cell counts. Lupus mainly affects neutrophils and lymphocytes, which are types of wbc. The severity of the disease can cause both lymphopenia (low lymphocyte counts) and neutropenia (low neutrophil counts) in SLE. Autoantibodies also play a role. These are antibodies that attack the body’s own cells. They can directly decrease neutrophil and lymphocyte counts in SLE.
Rheumatoid arthritis is another autoimmune condition. It can also lead to a low white blood cell count. In some cases, conditions like Felty’s syndrome or large granular lymphocyte syndrome, associated with rheumatoid arthritis, cause leukopenia. This happens due to antibody-mediated and cell-mediated cytotoxicity. This means the immune system’s antibodies and cells directly kill wbc. This can reduce the overall wbc.
Chronic Illnesses
Long-term health problems, or chronic illnesses, can also affect the white blood cell count. These conditions can impact how the body produces white blood cells. They can also increase how quickly the body removes white blood cells from circulation.
One way chronic illnesses cause a low white blood cell count is through hypersplenism. The spleen is an organ that filters blood. In hypersplenism, the spleen becomes enlarged and overactive. It traps and destroys blood cells, including wbc, more than it should. This leads to mild neutropenia. This happens because more wbc get stuck in the enlarged spleen.
Some chronic conditions can also lead to secondary autoimmune neutropenia. This means the body develops antibodies against its own neutrophils, a type of wbc. Conditions like Graves’ disease, Wegener’s granulomatosis, rheumatoid arthritis, or systemic lupus erythematosus can cause this. These anti-neutrophil antibodies can contribute to a low white blood cell count. However, the link between these antibodies and how severe the neutropenia is does not always appear strong.
Nutritional Deficiencies
A poor diet can significantly impact the body’s ability to produce white blood cells. Malnutrition or a lack of essential nutrients can impair both the production and activity of immune cells, including white blood cells. Aging often comes with micronutrient deficiencies. These deficiencies can worsen a decline in immune function. This can affect the production of immune cells by organs like the bone marrow.
Deficiencies in vitamin B12 and folic acid are directly linked to problems with neutrophils. Neutrophils are a type of wbc. These deficiencies cause changes in the shape and number of neutrophils. A study looked at patients with megaloblastic bone marrows.
These patients had vitamin B12 or folic acid deficiency. The study found that these patients’ neutrophils could still engulf bacteria (phagocytosis). However, their metabolic activation during phagocytosis was much lower in vitamin B12 deficient patients. Bacterial killing was also slightly reduced in vitamin B12 deficiency. Specific therapy reversed these problems. This shows vitamin B12 plays a direct role in normal cell function. This includes white blood cell production and activity.
Pancytopenia, which includes a low white blood cell count, caused by vitamin B12 deficiency is rare. One study looked at 201 patients with vitamin B12 deficiency. It reported that 5% of them had pancytopenia. Another study investigated vitamin B12 deficiency in patients who already had leukopenia and neutropenia due to infection. This study found that 17 out of 60 patients (28.3%) had vitamin B12 deficiency. This suggests a notable presence of B12 deficiency among people already experiencing a low white blood cell count. This also shows that nutritional issues can lead to a low wbc.
A decreased white blood cell count stems from various issues. These include infections, medications, bone marrow problems, and autoimmune conditions. Remember, a low wbc is a symptom, not a disease itself. Identifying the underlying cause for a low wbc is crucial for effective management. Your wbc count helps fight illness. If you suspect a low white blood cell count, consult a healthcare professional. They can assess your wbc. Early diagnosis and treatment are vital for maintaining overall health and preventing complications from a low wbc. A healthy wbc level protects you. Your wbc are important.
FAQ
What does a low wbc count indicate?
A low wbc count, or leukopenia, indicates the body has fewer white blood cells than normal. This condition suggests a weakened immune system. It means the body may struggle to fight off infections effectively. Doctors consider a low wbc count a symptom, not a disease itself.
What are common causes of a low wbc count?
Many factors cause a low wbc count. Infections, certain medications, and bone marrow problems are primary reasons. Autoimmune diseases and nutritional deficiencies also contribute. Each cause affects the body’s ability to produce or maintain healthy wbc.
Can infections cause a low wbc count?
Yes, infections often cause a low wbc count. Severe viral infections, like HIV, directly destroy wbc. Bacterial infections can deplete wbc rapidly as the body uses them to fight pathogens. Parasitic infections also impact wbc levels.
What role does the bone marrow play in wbc production?
The bone marrow produces all blood cells, including wbc. Problems within the bone marrow directly reduce the wbc count. Conditions like aplastic anemia or cancers such as leukemia disrupt normal wbc production. Environmental toxins also damage bone marrow cells, affecting wbc.
How do medications affect wbc levels?
Many medications affect wbc levels. Cancer therapies, like chemotherapy, damage bone marrow cells that produce wbc. Immunosuppressants reduce immune system activity, lowering wbc counts. Other drugs, including some antibiotics, can also cause a decrease in wbc.



