When you pass clear liquid from your bowel, it can be a concerning symptom. This means your stool appears watery and transparent, often without solid matter. While sometimes harmless, this type of diarrhea can signal serious underlying issues. You might experience severe diarrhea, or persistent diarrhoea, which needs prompt medical attention.
Many people seek medical help for this symptom due to infections, certain foods, medications, or other health conditions affecting your bowel. These symptoms can lead to dehydration. This type of diarrhea often indicates a problem with your bowel. These urgent causes explained here require your attention. Persistent diarrhoea is a serious form of diarrhea.
Key Takeaways
Clear liquid stool means your body passes mostly water. This can be a sign of serious health problems.
Infections, certain foods, and some medicines can cause clear liquid stool. Conditions like IBS, IBD, and Celiac Disease are also causes.
Seek urgent medical help if you have clear liquid stool with signs of dehydration, a high fever, or blood in your stool.
Persistent or explosive diarrhea needs quick medical attention. These symptoms can mean a serious problem.
Doctors will check your symptoms and history to find the cause. They will help you rehydrate and treat the main problem.
What is Clear Liquid Stool?
Clear liquid stool means you pass bowel movements that are mostly water. They lack solid matter. This differs from typical diarrhea, which can still have some solid or semi-solid components.When you experience watery diarrhea, your body loses more fluid than it absorbs.
This happens because your bowel cannot properly absorb solutes. Sometimes, your bowel actively secretes solutes into its lumen. This increases the fluid content in your stool. For example, insufficient solute absorption or active secretion of chloride ions can drive this.
Your intestine’s fluid secretion can overwhelm its absorptive capacity. This results in increased water loss. This leads to watery diarrhea. Your intestine’s ability to absorb fluid becomes overwhelmed. This leads to liquid stools. This type of diarrhea can be a symptom of various issues. This kind of watery diarrhea needs attention. This severe diarrhoea can quickly lead to dehydration.
Mucus in Bowel Movements
You might also notice mucus in your bowel movements. A small amount of mucus in your stool is normal. This mucus helps food and waste move through your intestines. It also protects your bowel from harmful bacteria. Normally, you do not see this mucus. If you do see it, it might appear clear, white, or yellow. It can look like stringy goop. Sometimes, it clings to the stool or appears in the toilet.
However, certain changes in mucus can signal problems. If you see increased amounts of mucus, or if it contains blood or pus, you should seek medical attention. White or yellow mucus can indicate underlying health issues.
For instance, Irritable Bowel Syndrome (IBS) often involves white or yellow mucus. These changes, especially with other gastrointestinal symptoms, are important symptoms. They can be signs of more serious conditions. Persistent diarrhoea with unusual mucus needs evaluation. This type of diarrhoea requires attention. This diarrhoea can be a sign of serious bowel problems.
Common Causes of Diarrhea
You often experience liquid bowel movements for several common causes. These causes range from temporary issues to chronic conditions. Understanding these causes of diarrhoea helps you know when to seek help.
Infections and Food Poisoning
Infection is a common cause of diarrhea, and gastroenteritis can result from a variety of infectious agents, including viruses, bacteria, and parasites. Viral gastroenteritis typically leads to watery diarrhea, with common viral pathogens such as Rotavirus, Norovirus, Adenovirus, and Astrovirus.
Bacterial infections are another frequent cause of acute diarrhea. Notable examples include Escherichia coli, Salmonella species, Shigella species, and Campylobacter species. Parasitic infections can also contribute to diarrheal illness. Giardia intestinalis commonly causes acute diarrhea with very watery stools, while Entamoeba histolytica can lead to bloody diarrhea accompanied by mucus. Other parasites, such as Cryptosporidium species, are also known to cause watery diarrhea.
Food poisoning occurs when contaminated food is consumed, often resulting in the sudden onset of watery diarrhea. Common foodborne pathogens include Campylobacter, Norovirus, and Salmonella. Campylobacter is a frequent bacterial cause of diarrhea, while Norovirus is a leading viral cause. Salmonella remains one of the most commonly reported bacterial causes of diarrheal disease in the United States. Certain strains of E. coli can also cause severe illness, beginning with mild abdominal discomfort or non-bloody diarrhea, and may rapidly progress to acute symptoms.
Foodborne gastrointestinal infections require prompt attention, as food poisoning represents a significant health concern.
Medications and Diet
Some medications can cause diarrhea as a side effect. Antibiotics are a common example. They can disrupt the natural balance of bacteria in your bowel. Other medications like antacids, PPIs, antidepressants, and chemotherapy drugs can also cause watery diarrhea.
Your diet also plays a big role. Food intolerances can trigger diarrhoea. For example, many people struggle to digest lactose found in dairy foods. Fructose, in fruits and artificial sweeteners like sorbitol, stimulates your gut. This releases water and loosens bowel movements.
Gluten, a protein in wheat, can cause digestive issues for sensitive individuals. Fried or fatty foods are hard to digest. Unabsorbed fats reach your colon. They prompt fluid secretion and watery diarrhea. Spicy foods and caffeine can also accelerate your digestive system. These dietary causes can lead to watery diarrhea.
Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a common bowel disorder. It affects your large intestine. IBS often involves recurrent abdominal pain. This pain occurs at least 1 day per week for the last 3 months. It is related to defecation. It also involves changes in stool frequency or form. You might experience diarrhea as a main symptom. This is called IBS with predominant diarrhoea (IBS-D). Your stool might appear as fluffy pieces with ragged edges or be entirely liquid. These are Bristol Stool Form Scale types 6 or 7. IBS is a chronic condition. It can cause significant discomfort and watery diarrhea. This acute diarrhoea can be challenging to manage.
Urgent Medical Causes Explained
You need to understand that some conditions causing clear liquid from your bowel are serious. These are urgent causes explained here. They require immediate medical attention. You should not ignore these symptoms.
Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) is a group of chronic conditions. They cause inflammation in your digestive tract. The two main types are Crohn’s disease and ulcerative colitis. Both can lead to severe diarrhea.
Inflammation is a primary factor. It causes diarrhea in IBD. This leads to abnormal intestinal ion transport and motor function. The severity and frequency of diarrhea depend on the degree, location, and extent of intestinal inflammation.
In ulcerative colitis, a main cause of liquid bowel movements is a big drop in sodium absorption. This also affects chloride and water absorption from your colon’s lumen. This malabsorption happens because the Na+/K+-adenosine triphosphatase (ATPase) pump in your colon cells works less. Apical sodium channels also do not work well.
You can see the prevalence of these conditions in different populations.
Population Group | Crohn’s Disease (per 100,000) | Ulcerative Colitis (per 100,000) |
|---|---|---|
Pediatric (age <20) – Overall | 57.8 | 33.9 |
Adult (age ≥20) – Overall | 241.3 | 263.0 |
Pediatric (age <20) – Northeast | 65.1 | 38.3 |
Pediatric (age <20) – South | 54.1 | 33.4 |
Pediatric (age <20) – Midwest | 61.4 | 31.5 |
Pediatric (age <20) – West | 43.2 | 31.1 |
Adult (age ≥20) – Northeast | 247.2 | 279.3 |
Adult (age ≥20) – South | 219.2 | 226.1 |
Adult (age ≥20) – Midwest | 264.0 | 275.0 |
Adult (age ≥20) – West | 219.3 | 263.9 |
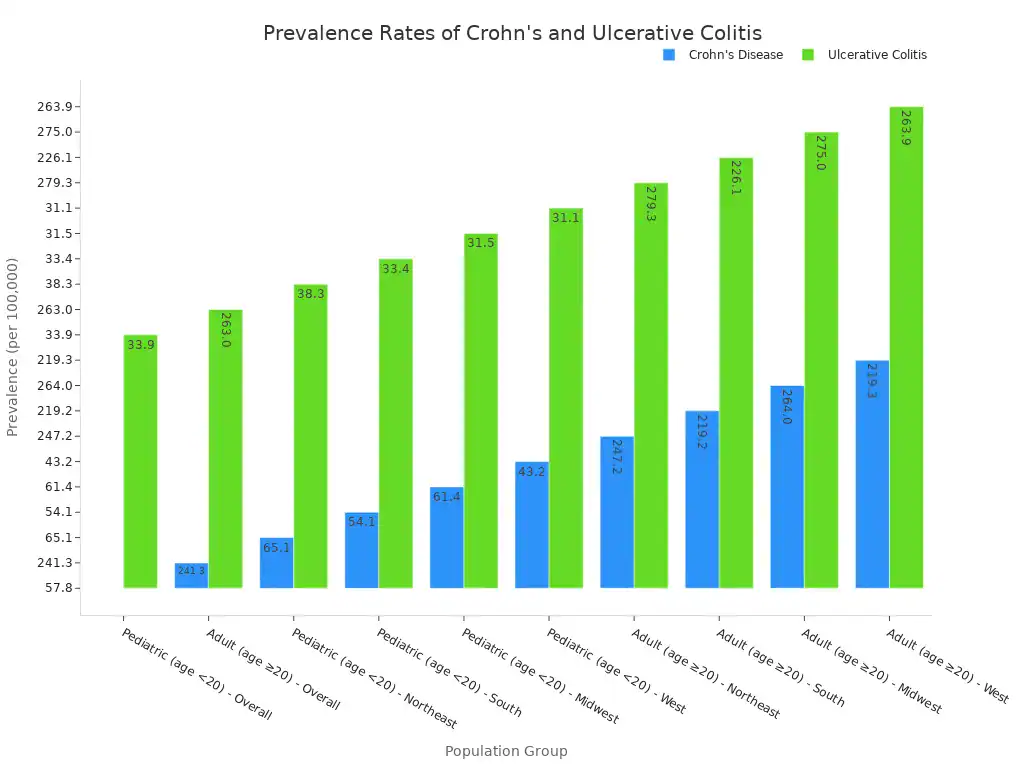
Prevalence rates for both Crohn’s disease and ulcerative colitis show significant regional variation. You see lower rates in the South and West compared to the Northeast and Midwest. Pediatric ulcerative colitis is an exception. Only the Northeast had a significantly higher prevalence for this group.
Sex-specific differences also exist. Pediatric Crohn’s disease was lower in girls than boys. Adult Crohn’s disease was higher in women. Ulcerative colitis showed no significant sex difference in either age group. If you have inflammatory bowel disease, you might experience chronic diarrhoea.
Celiac Disease and Malabsorption
Celiac Disease (CD) is an autoimmune disorder. It affects your small intestine. You cannot eat gluten if you have this condition. Gluten is a protein found in wheat, barley, and rye. When you eat gluten, your immune system attacks your small intestine. This damages the lining.
This damage leads to malabsorption. Malabsorption means your body cannot properly absorb nutrients. This can cause watery diarrhea.
The global prevalence of Celiac Disease is 1%. Its prevalence has significantly increased over the last 50 years. Many people with CD remain undiagnosed. This is due to varied symptoms or a lack of awareness among medical professionals.
Celiac Disease has a worldwide prevalence of 1%. A higher incidence is observed in women. Historically underestimated, CD is now recognized as one of the most common genetic disorders in Western populations. The male-to-female ratio is approximately 1:2.8.
When you have malabsorption, it contributes to clear liquid stool.
When bile salts are not properly absorbed in your ileum, they reach your colon. Their presence in your colon triggers the secretion of large amounts of fluid. This directly contributes to watery diarrhea. This can show as clear liquid stool.
Malabsorption, especially of carbohydrates, leads to clear liquid stool. This happens primarily through osmotic fluid retention. Unabsorbed carbohydrates, along with organic acids and electrolytes, create an osmotic load. This draws fluid into your colon. This increased fluid volume, combined with the osmotic effect, speeds up colonic transit. This results in watery diarrhea.
Doctors use several tests to diagnose Celiac Disease:
Common Serologic Tests: Anti-endomysial antibody (EMA) and anti-tissue transglutaminase (tTG) are widely used.
Modern Test: Anti-deamidated gliadin peptide is a reliable test. It has greater sensitivity and specificity. However, doctors use it less commonly than EMA and tTG.
Less Used Tests: Anti-gliadin antibodies are not frequently used. This is due to their poor sensitivity and specificity.
Your initial evaluation combines several factors:
Positive CD-specific serological tests.
Histological findings from intestinal biopsies.
Presence of CD-predisposing HLA DQ2 or DQ8 genes.
Family and medical history.
Clinical or histological response to a gluten-free diet (GFD).
Genetic Markers: Almost all CD patients carry HLA-DQ2 or HLA-DQ8. Their absence indicates a very high negative predictive value for CD.
Serological Markers: Positive tissue transglutaminase (TGA) or endomysial antibodies (EMA) at diagnosis or during the disease course confirm CD. This is especially true with small bowel villous atrophy. Their specificity exceeds 99%.
Histological Findings: Small intestinal mucosal histology is the diagnostic gold standard. It shows typical architectural abnormalities. Marsh’s progression theory describes these.
Aberrant Intraepithelial Lymphocytes (IELs): The presence of aberrant IELs can differentiate between RCD type I and type II. It is associated with increased EATL development. They can support or exclude CD diagnosis. They also aid follow-up.
Serum Antibodies: EMA and TGA offer superior sensitivity and specificity (over 95% when combined) compared to anti-gliadin antibodies (AGA). Deamidated gliadin peptide AGA (DGP-AGA) shows improved accuracy. IgA DGP-AGA has 84.3% sensitivity and 79.8% specificity. IgG DGP-AGA has 82.3% sensitivity and 98.9% specificity. EMA testing is subjective. TGA testing is quantitative.
Bowel Obstruction
A bowel obstruction happens when something blocks the normal passage of food and liquids through your bowel. These blockages can be:
Location-based: In your small intestine or your large intestine.
Severity-based: Partial (some feces can still pass) or complete (fully blocked, preventing even gas from passing).
Complication-based: Simple (just a blockage) or complicated (the blockage has cut off your bowel‘s blood supply, causing damage).
Common causes of bowel obstruction in adults include:
Adhesions: Scar tissue often forms after abdominal or pelvic surgery. This can cause your bowel to twist.
Bowel cancer.
Hernias. Other potential causes are:
Inflammatory bowel disease like Crohn’s disease or Ulcerative Colitis.
Diverticulitis.
Volvulus (your bowel twisting on itself).
Intussusception (your bowel folding into itself, more common in infants and young children).
Foreign bodies, such as swallowed objects or gallstones.
Severe constipation.
A pseudo-obstruction, or functional bowel obstruction, differs from a mechanical obstruction. It involves improper muscle contractions in your bowel without a physical blockage. Its possible causes include:
Abdominal surgery.
Injuries.
Muscle or nerve disorders.
Abdominal infections.
Certain medications, such as opioids.
Low potassium levels. You might experience watery diarrhea around the obstruction. This is called overflow diarrhoea.
Fecal Incontinence
Fecal incontinence means you cannot control your bowel movements. This can result in passing clear liquid from your bowel. It is a distressing condition. Several causes contribute to it.
Diarrhea
Constipation
Tear or separation of your anal sphincter
Muscle damage (e.g., during childbirth)
Nerve damage (e.g., due to diabetes, Parkinson’s disease, stroke)
Weakness of your anal sphincter complex
Other causes include:
Muscle damage (often from childbirth)
Older age
Nerve damage
Rectal prolapse
Chronic diarrhoea
Inflammatory bowel disease
Surgery
Long-term conditions can also lead to fecal incontinence. These include diabetes, multiple sclerosis, and dementia. Physical problems with the body parts controlling your bowel can also cause it. Problems with your rectum mean you cannot retain stool.
Problems with your sphincter muscles mean they malfunction. Nerve damage means signals from your rectum do not reach your brain. Constipation can lead to fecal impaction and weakened rectal muscles. This can result in overflow diarrhoea. These are all urgent causes explained that require medical attention.
When to Seek Urgent Care

You must recognize specific red-flag symptoms that necessitate immediate medical consultation. Ignoring these signs can lead to serious health complications. You need to understand when your clear liquid from the bowel indicates an emergency.
Signs of Severe Dehydration
Clear liquid diarrhea can quickly lead to dehydration. You lose essential fluids and electrolytes. Severe dehydration is a critical condition. You must seek urgent medical care if you notice these signs.
You might experience extreme thirst. Your breathing can become fast, and your heart rate might increase. You could also have low blood pressure. You may feel irritable, tired, or confused. Your hands and feet might feel cold. Your eyes could appear sunken. If you observe these signs of dehydration, you need help.
For babies, a sunken fontanelle (the soft spot on their head) is a key indicator. You might also notice extreme tiredness or lethargy. They could have rapid or quick breathing. They might cry without tears. You might feel dizzy or unable to stand. They may not urinate for over 12 hours. You could even pass out. These are all critical signs of dehydration.
Other signs of dehydration include:
Lack of urination or very dark yellow/amber urine.
Dry, shriveled skin.
Irritability or confusion.
Dizziness or lightheadedness.
Rapid heartbeat.
Rapid breathing.
Sunken eyes.
Listlessness.
Shock (insufficient blood flow).
Unconsciousness or delirium.
You must act quickly if you see these signs of severe dehydration.
Fever and Blood
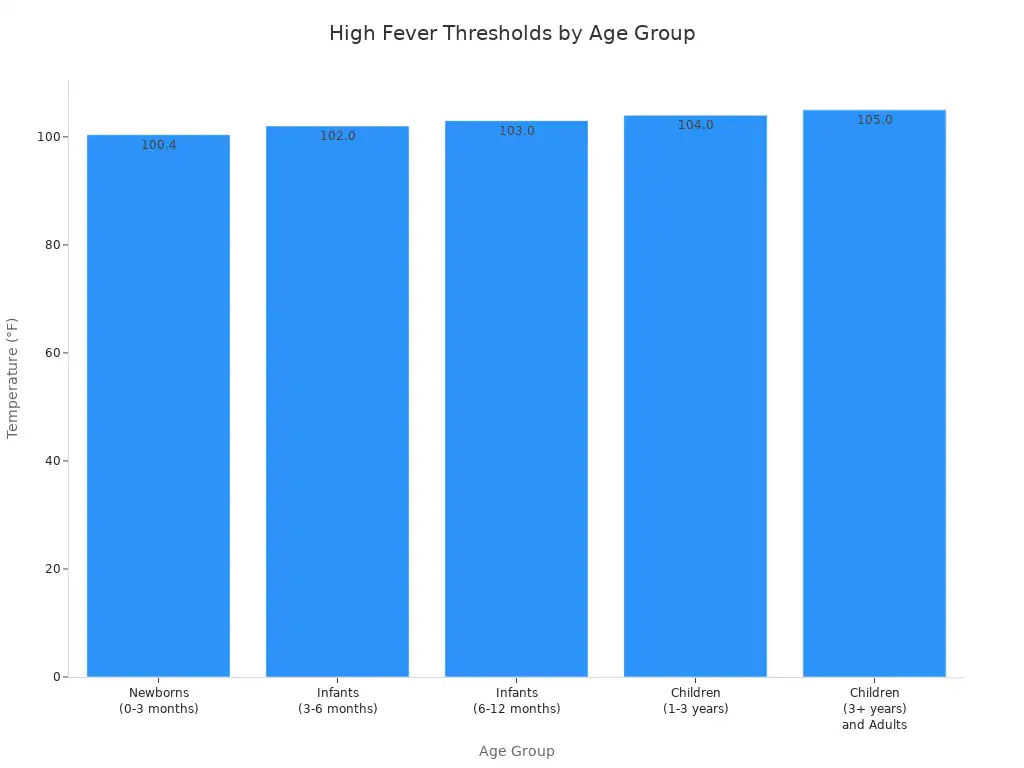
A high fever accompanying diarrhea is a serious symptom. You need to know what temperature thresholds indicate an urgent situation.
Age Group | Temperature Threshold | Accompanying Symptoms Warranting Urgent Care |
|---|---|---|
Newborns (0-3 months) | Rectal temperature of 100.4°F (38°C) or higher | Any fever in this age group requires immediate medical attention. |
Infants (3-6 months) | Rectal temperature of 102°F (38.9°C) or higher | Irritability, lethargy, poor feeding, difficulty breathing, rash, or any other concerning symptoms. |
Infants (6-12 months) | Rectal temperature of 103°F (39.4°C) or higher | Persistent fever, extreme fussiness, decreased wet diapers, signs of dehydration, difficulty breathing, rash, or any other concerning symptoms. |
Children (1-3 years) | Oral temperature of 104°F (40°C) or higher | Fever lasting more than 24-48 hours, lethargy, severe headache, stiff neck, difficulty breathing, rash, signs of dehydration, or any other concerning symptoms. |
Children (3 years and older) and Adults | Oral temperature of 105°F (40.6°C) or higher | Fever lasting more than 72 hours (3 days), severe headache, stiff neck, confusion, difficulty breathing, chest pain, abdominal pain, rash, seizures, signs of dehydration, or any other concerning symptoms. |
Any Age Group | Any temperature | If accompanied by severe symptoms such as difficulty breathing, severe headache, stiff neck, confusion, seizures, unexplained rash, persistent vomiting or diarrhea, signs of dehydration, or if the individual has a compromised immune system or a chronic medical condition. |
You should also watch for blood in your stool. This is a significant red flag. You might see bright red blood, dark red blood, or black, tarry stools. Black stools often indicate bleeding higher in your digestive tract.
You must contact your care team if you see blood of any shade.
Other urgent symptoms include:
Fever.
Excessive weakness.
Vomiting.
Large amounts of blood in your stool.
These symptoms, especially with acute diarrhoea, demand immediate medical attention.
Persistent or Explosive Diarrhea
You need to monitor the duration and nature of your diarrhea. Persistent diarrhea or explosive diarrhea can signal serious underlying conditions.
Diarrhea is persistent if it lasts between 14 and 30 days. You should seek medical evaluation if symptoms of infectious diarrhea persist for seven days or more. This often starts with molecular or antigen testing. For general diarrhea, an endoscopic evaluation is typically not required unless symptoms continue for over a month and initial laboratory results are inconclusive. This prolonged acute diarrhoea can lead to severe dehydration.
Explosive diarrhea is another urgent concern. This type of watery diarrhea comes on suddenly and forcefully. It can quickly lead to dehydration.
You should seek medical care if you experience explosive diarrhea with these characteristics:
Diarrhea lasting longer than two days (or 24 hours in a child).
Signs of dehydration, such as excessive thirst, dry mouth, reduced urination, or dizziness.
Blood or pus in the stool, or black-colored stool.
A high fever: 101.5 °F (38.6 °C) or greater in an adult, or 100.4 °F (38 °C) or higher in a child.
Severe abdominal or rectal pain.
Diarrhea occurring at night.
Chronic diarrhea, defined as lasting more than four weeks, requires medical investigation.
Hemolytic Uremic Syndrome (HUS) is a serious complication. It presents with specific symptoms of diarrhoea:
Severe diarrhea, which may be bloody.
Fever.
Abdominal pain.
Vomiting.
Decreased urination.
Bruising.
You must not delay seeking medical help for these symptoms. Your health depends on prompt action.
Diagnosis and Treatment
You need proper diagnosis and effective treatment when you pass clear liquid from your bowel. This helps address the underlying causes and manage your symptoms.
Medical Evaluation
Your doctor will start with a thorough medical evaluation. They will ask about your symptoms, including the duration of your diarrhea and how your stool looks. You will discuss your eating and drinking habits.
You should mention any recent international travel. Your family history is also important. This includes any digestive tract problems, food allergies, or conditions like celiac disease or irritable bowel syndrome. This comprehensive approach helps identify the specific causes of your diarrhea.
Rehydration and Management
Managing clear liquid diarrhea often involves rehydration. You must replace lost fluids and electrolytes. Oral rehydration solutions (ORS) are crucial. These solutions contain water, glucose, sodium chloride, sodium citrate, and potassium chloride. This specific mix helps your intestines absorb fluid better.
Glucose helps your body take in sodium and water. Potassium chloride and sodium citrate prevent issues like low potassium and acidosis. For healthy adults, you can often start rehydration by drinking water, clear broth, diluted juices, or sports drinks. If you have severe dehydration, you need immediate intravenous fluid treatment. This is a medical emergency. This rehydration is vital to your recovery.
Treating the Underlying Cause
Your treatment plan will target the specific cause of your diarrhea. For bacterial infections, your doctor might prescribe antibiotics. However, empiric antimicrobial treatment is generally not recommended for most adults with bloody diarrhoea unless specific exceptions apply. These exceptions include infants under 3 months, very ill individuals with high fever, or those with recent international travel. Your doctor will choose the right treatment.
They might use a fluoroquinolone or azithromycin for adults. For children, a third-generation cephalosporin or azithromycin might be used. You should avoid antibiotics if your infection is due to certain E. coli strains that produce Shiga toxin. This treatment approach ensures you get the right care for your acute diarrhoea.
Do not ignore clear liquid from your bowel, especially with other concerning symptoms. Many urgent causes explained in this blog can lead to severe diarrhea. Recognize red flags like fever or blood in your bowel movements. These are serious symptoms.
Consult a healthcare professional for accurate diagnosis and treatment. Self-diagnosis for persistent diarrhoea is dangerous. Many causes of diarrhoea exist. You need proper care for your bowel. This includes understanding different types of diarrhoea. Chronic diarrhoea affects your bowel health. Acute diarrhoea can also be serious. This severe diarrhoea can indicate a problem with your bowel. Proactively manage your health to prevent serious diarrhea and other diarrhoea.