Yes, a terrible bad argument can indeed contribute to a stroke, though it’s not a direct ’cause’ in isolation. Intense emotional upset and anger, often associated with a bad argument, have been identified as significant triggers for stroke, particularly in susceptible individuals. Acute emotional distress increases the risk of stroke. Stress increases cerebrovascular disease risk by modulating sympathetic activity. It affects blood pressure reactivity, the cerebral endothelium, coagulation, and heart rhythm. These physiological changes can elevate an individual’s risk of stroke. Understanding these emotional triggers helps explain how underlying health conditions interact with an acute emotional state to elevate health risk.
Key Takeaways
Strong emotions like anger can trigger a stroke, especially for people already at risk. These emotions cause changes in the body that make a stroke more likely.
Anger and emotional upset can increase your risk of having a stroke within an hour. This is because stress hormones affect your blood vessels and heart.
People with existing health problems like high blood pressure or diabetes are more likely to have a stroke from emotional triggers. Long-term stress also increases this risk.
Managing anger and stress can help prevent a stroke. Use deep breathing, therapy, and relaxation to keep your body calm.
Eating healthy foods and taking care of your heart also lowers your stroke risk. These actions protect your blood vessels and overall health.
The Link Between a Bad Argument and Stroke Risk

A clear scientific connection exists between intense emotional distress and an elevated risk of stroke. Research shows that strong feelings, especially negative ones, can directly influence the body in ways that make a stroke more likely. This is not just about feeling stressed; it involves specific physiological changes that increase vulnerability.
Acute Emotional Upset as a Trigger
Sudden, intense emotional upset can act as a direct trigger for an acute stroke. Studies have explored how different emotional states connect to stroke risk. For example, a Mendelian randomization study found that low satisfaction with family relationships increased the risks of all stroke types and ischemic stroke. Mood swings also linked to higher risks of all stroke, ischemic stroke, and large-artery stroke. Feelings of tension showed an association with large-artery stroke and small vessel stroke. These findings highlight how various emotional states can contribute to stroke risk.
When someone experiences acute emotional upset, their body undergoes several changes. The sympathetic nervous system becomes highly active. This leads to increased catecholamine excretion, which are stress hormones. Blood vessels constrict, meaning they narrow. In some cases, feelings of upset can even cause cardiac arrhythmia, an irregular heartbeat. These physiological responses put extra strain on the cardiovascular system, potentially leading to an acute stroke.
Increased Risk After Anger
Anger is a particularly strong emotional trigger for stroke. Experiencing anger or emotional upset significantly raises the risk of stroke. Research indicates that anger or emotional upset is linked to an approximately 30% higher risk of having a stroke within one hour of experiencing those emotions. This means the immediate aftermath of an intense emotional event, like a bad argument, carries a notable risk.
The INTERSTROKE study, a large international study, provided strong evidence for this link. It involved over 13,000 patients. This study found that anger or emotional upset within one hour of stroke symptoms increased the odds of all stroke types. Specifically, it increased the odds of ischemic stroke and intracerebral hemorrhage. This shows that anger and other negative emotions can trigger different kinds of stroke. Following an angry outburst, an individual faces an increased risk of a cardiovascular event, such as a stroke, especially within the first two hours. Furthermore, the ability of blood vessels to dilate, which is crucial for healthy blood flow, can remain impaired for up to forty minutes after an anger-inducing event before returning to normal. This temporary impairment adds to the overall risk.
How Emotions Impact the Body

Emotional triggers can significantly affect the body’s internal systems. These physiological changes explain how an intense emotional state can contribute to a stroke. The body reacts to stress in specific ways, impacting various functions.
Physiological Responses to Stress
Acute psychological stress activates the body’s “fight or flight” response. This response involves several immediate changes. The heart rate increases right away. Heart rate variability typically decreases during this time. The sympathetic nervous system becomes highly active. This system modulates blood glucose levels, body temperature, cardiac output, and immune system function. Blood flow increases to skeletal muscles, the heart, and the brain. Pupils dilate. The liver releases more glucose into the blood. Adrenaline and noradrenaline mediate these responses. They boost heart rate and breathing. They also constrict blood vessels. These responses prepare the body for perceived danger.
Stress hormones play a crucial role in these reactions. They can have direct effects on vascular health.
Noradrenaline (norepinephrine): Arterial walls release noradrenaline. It directly stimulates α-adrenergic receptors. This leads to endothelial dysfunction. It also promotes hematopoietic stem cell proliferation. This increases the release of leukocytes. These leukocytes migrate to arterial walls and atherosclerotic plaques. This contributes to inflammation and plaque rupture.
Corticotropin-releasing hormone (CRH): The hypothalamus releases CRH within seconds of stress. It contributes to endothelial dysfunction. It does this by stimulating the release of the vasoconstrictor ET-1 from the endothelium.
Cortisol: The body releases cortisol 20–40 minutes after stress begins. It impairs endothelial function. It inhibits nitric oxide (NO) synthesis. It also increases ET-1 release. Chronic exposure to high cortisol levels can induce resistance. This reduces its anti-inflammatory actions. It increases inflammatory cytokines. This leads to perivascular inflammation, endothelial dysfunction, and progression of coronary artery calcification.
Epinephrine (catecholamine): Acute emotional stress can cause severe catecholamine release. This leads to direct myocyte injury due to calcium overload (myocytolysis). It also causes coronary microvascular vasoconstriction. It increases left ventricular afterload. These changes can trigger stress (Takotsubo) cardiomyopathy.
These stress hormones significantly increase the risk of adverse cardiovascular outcomes.
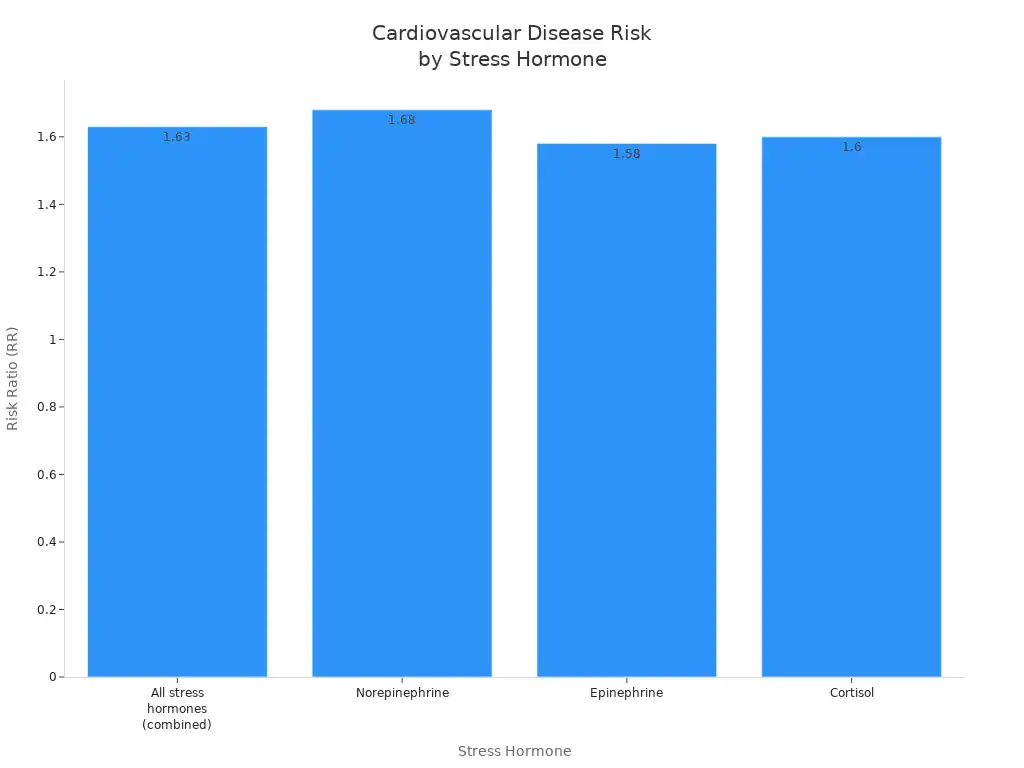
Stress Hormone | Risk Ratio (RR) for Cardiovascular Diseases (compared to lower levels) |
|---|---|
All stress hormones (combined) | 1.63 (95% CIs: 1.36, 1.97) |
Norepinephrine | 1.68 (95% CIs: 1.37, 2.06) |
Epinephrine | 1.58 (95% CIs: 1.10, 2.26) |
Cortisol | 1.60 (95% CIs: 1.04, 2.26) |
Blood Vessel Function and Stroke
Blood pressure spikes are a key mechanism connecting emotional triggers to stroke. High blood pressure damages blood vessels over time. This makes them more susceptible to blockages or rupture. Uncontrolled hypertension can lead to blood clot formation. These clots can obstruct blood flow to the brain. This causes an ischemic stroke. High blood pressure also weakens blood vessel walls. This increases the likelihood of a hemorrhagic stroke.
Dynamic blood pressure changes provide critical information for predicting stroke risk. This is because vascular damage leading to stroke is complex and dynamic. Traditional analyses based on single measurements may underestimate the true relationship between elevated blood pressure and disease.
High blood pressure causes blood to flow with excessive force through arteries. This leads to damage.
This damage can result in ‘hardening of the arteries’ (arteriosclerosis).
Specific types of vascular injury contribute to stroke:
Atherosclerosis: Plaque builds up in larger arteries. Plaque contains fatty substances, cholesterol, and waste products. This reduces blood flow. If a piece of plaque breaks off and blocks blood flow in the brain, it causes a stroke.
Arteriolosclerosis: This affects smaller arteries (arterioles). High blood pressure stiffens these arterioles. This leads to blockages. It can also weaken them, making them prone to tears and rupture.
Excessive force from high blood pressure stretches arteries beyond their healthy limit. This causes small tears. The body initiates an injury-healing response. It forms scar tissue to repair these tears. This scar tissue traps substances that form plaque. Plaque can lead to blockages, blood clots, and hardened, weakened arteries.
Ischemic strokes: These occur when a blood clot or plaque blocks an artery supplying blood to the brain. They account for nearly 90% of strokes.
Hemorrhagic strokes: These result from a weakened blood vessel in the brain tearing. Constant high blood pressure causes this tearing. It leads to bleeding inside or around the brain. These strokes are often more damaging and harder to treat.
Short periods of anger have been observed to lead to impaired blood vessel function. The precise reasons or mechanisms behind these changes are not yet fully understood. Further investigation into these underlying connections between anger and blood vessel dysfunction is needed. This will help identify potential intervention strategies for individuals at higher risk of cardiovascular issues. While anger negatively impacts blood vessel function, the specific mechanisms remain unclear. Researchers hypothesize several factors could contribute. These include the activation of the autonomic nervous system, alterations caused by stress hormones, and increased inflammation within the arteries. The endothelium, the inner lining of blood vessels, plays a crucial role in controlling their dilation. It is also thought to be involved. Future studies will explore these potential mechanisms in more detail. These negative emotions can significantly impact vascular health.
Who is Most Vulnerable to Stroke?
Certain individuals face a higher risk of stroke when exposed to emotional triggers. Understanding these vulnerabilities helps people protect their health. Several risk factors make someone more susceptible to an acute stroke after an intense emotional event.
Identifying Underlying Risk Factors
People with pre-existing cardiovascular conditions are particularly vulnerable. These conditions include high blood pressure, high cholesterol, and diabetes. Elderly patients also have a higher risk because their bodies are often less resilient to sudden stress. Socioeconomic status and where a person lives also play a role.
Low socioeconomic status (SES) increases the negative impact of psychological distress on mortality from stroke and cardiovascular disease. This suggests a combined effect rather than just an added one.
Low job control linked to stroke risk in women in lower-status manual jobs.
Job strain correlated with higher stroke chances in men from lower professional classes.
Job demands accentuated socioeconomic differences in cerebrovascular disease.
Effort-reward imbalance was particularly harmful to coronary health in individuals with the lowest employment grades.
Work-related stress associated with angina pectoris, especially in men and women with low educational levels or occupational positions.
Increased coronary health risk among lower occupational class working women partly explained by multiple sources of work and non-work stress.
Lower SES individuals may cope less effectively with stress. They often have smaller support networks and fewer material resources. Biobehavioral differences, such as slower cardiovascular recovery after acute stroke in lower SES categories, also contribute to disease progression.
Chronic Stressors and Vulnerability
Long-term stressors significantly increase vulnerability to stroke. Chronic work pressure, sleep deprivation, poor diet, and anxiety all contribute to this elevated risk.
Chronic sleep deprivation has several negative effects:
Increased inflammation.
Endothelial dysfunction.
Heightened blood pressure.
Metabolic dysregulation.
Heightened sympathetic nervous system activation, which increases vascular stress.
Disruption of the hypothalamic–pituitary–adrenal axis, leading to higher cortisol levels.
Impaired glymphatic system function, affecting brain health.
These issues contribute to obesity, impaired glucose metabolism, hypertension, and dyslipidemia. Shift work also disrupts normal circadian rhythms, leading to elevated blood pressure and an increased risk of cardiovascular problems. Rotating night shift work is associated with a 4% increased risk of stroke for every five years of exposure.
Higher anxiety levels are associated with an increased long-term risk of incident stroke. This association remains significant even after controlling for depression. Every 1 SD increase in anxiety links to a 17% increase in stroke risk. Behavioral factors like smoking and physical activity explain some of this link. However, direct biological effects of anxiety also play a role. Chronic anxiety can lead to excess activation of stress systems, potentially increasing stroke risk. Anxiety might also contribute to stroke by lowering the threshold for arrhythmia. Managing emotions like anger and anxiety is crucial for overall health.
Managing Emotional Triggers and Preventing Stroke
People can actively manage emotional triggers to reduce their risk of stroke. Adopting healthy coping mechanisms and making lifestyle adjustments are crucial steps. These actions protect both physical and mental health.
Strategies for Anger Management
Managing anger effectively helps mitigate stroke risk. Deep breathing exercises calm the nervous system and reduce physiological arousal. Cognitive Behavioral Therapy (CBT) helps individuals identify and change negative thought patterns that fuel anger. CBT also teaches people to recognize anger triggers.
It helps them replace irrational thoughts with balanced perspectives. Individuals learn coping skills like counting or deep breathing to manage emotional responses. Relaxation techniques, such as progressive muscle relaxation or guided imagery, calm the mind and body. Mindfulness and meditation enhance emotional awareness.
They decrease impulsive reactions. Physical activity releases tension and boosts mood-enhancing endorphins. Assertive communication allows clear expression of feelings without blame. Problem-solving skills address the root causes of anger constructively. For chronic anger or stress, seeking professional help is important for long-term mental health and overall health. CBT interventions can lessen health risks linked to high trait anger.
Promoting Overall Cardiovascular Health
Promoting overall cardiovascular health significantly reduces stroke risk. Relaxation techniques effectively manage stress. Treating mood disorders, like depression, is also vital. Mindfulness-based therapies, such as mindfulness meditation, improve psychological problems in patients with vascular diseases. Mind-body techniques, like Transcendental Meditation (TM), lower blood pressure. They reduce the risk of myocardial infarction, stroke, and mortality in patients with coronary artery disease.
Diet plays a critical role in vascular health. The Mediterranean diet, rich in olive oil, whole grains, fruits, vegetables, and legumes, strongly supports stroke prevention. People should limit animal flesh and seldom consume red meat. Avoiding egg yolks is also recommended for stroke prevention.
High intake of vegetables, fruits, and legumes is beneficial. Individuals should avoid deep-fried foods, hydrogenated oils, sugar, and refined grains. Incorporating nuts, herbs, and spices can further reduce cardiovascular risk. Soluble fiber from foods like oatmeal and beans supports gut health and lowers cholesterol. Potassium-rich foods help lower blood pressure. Limiting salt and sugar intake also protects cardiovascular health. These dietary changes contribute to better health and reduce the risk of stroke.
A bad argument does not directly cause a stroke. However, intense emotional stress it generates can trigger an acute stroke, especially for individuals with existing risk factors.
Emotional stress, particularly chronic anger from a bad argument, contributes to both acute stroke events and long-term cardiovascular disease risk. Managing emotional well-being and stress is vital for good health. Proactive health measures are crucial components of stroke prevention. They support overall cardiovascular health and reduce stroke risk. Understanding these emotional triggers and acute responses is key to reducing stroke risk factors. Prioritizing emotional health reduces stroke risk.




