Bile is a vital digestive fluid. The liver produces bile, and the gallbladder stores it. Bile helps the body break down fats and absorb essential nutrients. However, problems arise with excess bile production. This often means bile is not overproduced.
Instead, issues like malabsorption or reflux cause an excess of bile in the wrong places. Digestive discomfort and diagnostic challenges often accompany these bile-related issues. For instance, bile acid diarrhea affects about 1% of the general population.
This figure rises to 25% to 50% for individuals with functional diarrhea or IBS-D. This blog explores the causes, diverse symptoms, and effective relief strategies for excess bile production.
Key Takeaways
Excess bile often means bile is in the wrong place, not that the liver makes too much. This can cause problems like malabsorption or reflux.
Common signs of too much bile include frequent diarrhea, stomach pain, and bloating. Dark urine or yellow skin can also be signs.
Doctors use special tests like the SeHCAT test to find bile problems. They also ask about your symptoms and health history.
You can manage excess bile with medicines that bind bile acids. Eating less fat and more fiber also helps. Avoid foods that make your symptoms worse.
Bile’s Role and Excess Production
What Is Bile and Its Function:
Bile is a vital digestive fluid. The liver produces bile, and the gallbladder stores it. Bile helps the body break down fats and absorb essential nutrients. It plays several crucial roles in digestion.
Bile acts as a surfactant. It helps emulsify lipids in food. This means bile forms micelles around fat droplets. This process stops fat droplets from clumping together. It also increases the surface area for enzymes to digest fats.
Bile is crucial for absorbing fat-soluble substances. These include vitamins A, D, E, and K. Bile helps break down and absorb these fats.
Beyond digestion, bile serves as an excretion route for bilirubin. Bilirubin is a byproduct from the recycling of red blood cells by the liver. The liver constantly makes bile. A healthy liver ensures proper bile flow. The liver also processes toxins. Problems with the liver can affect bile. The liver works hard.
Defining Excess Bile Production:
Defining excess bile production involves understanding more than just the liver making too much bile. It means bile ends up in places it should not be. This can happen due to issues with bile acid malabsorption (BAM) or bile reflux. These conditions lead to an excess of bile in inappropriate locations.
For example, bile might be in the colon, stomach, or esophagus. This is not always about the liver making too much bile. Instead, problems with bile movement cause it. The liver’s health is key to this process.
Causes of Excess Bile Production
Various factors lead to excess bile in the digestive tract. These factors include conditions causing overproduction, malabsorption, or reflux. Understanding these causes helps in finding the right treatment.
Bile Acid Malabsorption (BAM):
Bile acid malabsorption (BAM) occurs when the small intestine does not properly absorb bile acids. This sends too much bile into the colon. The excess bile in the colon causes irritation and diarrhea. This condition is a common cause of chronic diarrhea.
Type 1 Bile Acid Malabsorption: This type often follows ileal resection or ileal inflammation, such as Crohn’s disease.
Type 2 Bile Acid Malabsorption (Idiopathic/Primary Bile Acid Diarrhea): This may result from an overproduction of bile acids. Lower levels of fibroblast growth factor 19 (FGF19) can increase bile acid synthesis.
Type 3 Bile Acid Malabsorption: Various gastrointestinal diseases cause this type. These include cholecystectomy, vagotomy, small intestinal bacterial overgrowth (SIBO), radiation enteropathy, celiac disease, and chronic pancreatitis.
BAM is a significant cause of chronic diarrhea. Its prevalence varies among patient groups.
Patient Group | SeHCAT at 7 days, % | BAM Prevalence, % |
|---|---|---|
Idiopathic chronic diarrhea | <15 | 27.0 |
IBS-D, postcholecystectomy | <8 | 39 |
Chronic diarrhea secondary to HIV infection | <15 | 84.2 |
Idiopathic chronic diarrhea | <10 | 44.7 |
IBS-D | <10 | 33.5 |
Idiopathic chronic diarrhea | <15 | 56 |
Chronic watery diarrhea | <11 | 59.7 |
IBS-D | <5 | 10 |
IBS-D | <10 | 32 |
IBS-D | <15 | 26 |
Idiopathic chronic diarrhea | <15 | 59.6 |
IBS-D | <10 | 39.2 |
Idiopathic chronic diarrhea | <15 | 50.9 |
IBS-D | <15 | 27.3 |
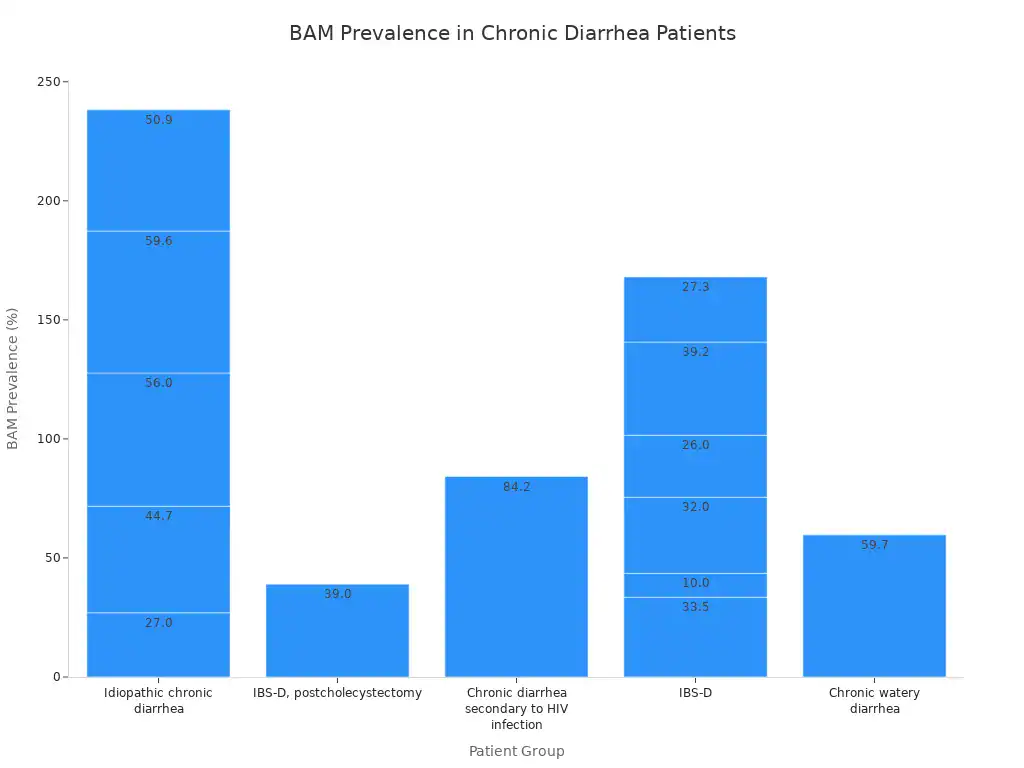
A systematic review of 18 studies found that 10% of patients with IBS-D had severe bile acid diarrhoea. About 32% had moderate to severe bile acid diarrhoea. Another 26% had some degree of bile acid diarrhoea.
Bile Reflux Conditions:
Bile reflux happens when bile flows backward from the small intestine into the stomach and esophagus. This causes irritation and inflammation. Bile reflux significantly amplifies risks associated with chronic gastroesophageal acid reflux (GERD).
Bile reflux gastritis links to stomach cancer.
Gastroesophageal Reflux Disease (GERD) symptoms may persist despite acid-suppressant medications. This suggests bile involvement.
Barrett’s esophagus is a serious condition. Long-term exposure to stomach acid and bile damages the esophageal lining. This increases cancer risk.
Esophageal cancer has a documented link with both acid and bile reflux.
Gallbladder and Liver Dysfunction:
The liver produces bile, and the gallbladder stores it. Problems with either organ affect bile flow and composition. When the gallbladder does not function properly, it affects fat digestion. Without proper bile release, fats remain undigested in the stomach longer. This can worsen GERD symptoms. Gallstones form when the gallbladder does not empty completely or often enough. This indicates a problem with bile storage and emptying.
Certain liver conditions also alter bile production.
Bile Acid Synthesis and Metabolism Defects: Genetic changes prevent the body from producing normal enzymes for bile acid synthesis. This leads to incorrectly formed bile acids and impaired liver function.
Peroxisomal Diseases: Conditions like Zellweger Syndrome disrupt bile acid production. Defects in the peroxisome part of the cell affect crucial steps. This can lead to varying degrees of liver damage. Liver cirrhosis is a specific liver condition. It changes bile acid composition and their overall pool. Chronic liver diseases, including cirrhosis, interact with the intestinal environment. They alter bile acid composition. This can contribute to bile-related liver diseases.
Post-Surgical Factors:
Some surgeries can lead to excess bile production or reflux.
Gastric Sleeve (Sleeve Gastrectomy): This procedure removes a large portion of the stomach. It can increase stomach pressure. This potentially weakens the lower esophageal sphincter. It leads to bile reflux.
Gastric Bypass (Roux-en-Y): This surgery can cause bile reflux in some patients. New connections between the stomach pouch and small intestine are the reason.
Gallbladder Removal (Cholecystectomy): After gallbladder removal, bile continuously trickles into the small intestine. There is no storage for bile. This increases the likelihood of bile reflux into the stomach. This continuous flow can also lead to large-scale movement of bile into the colon, causing bile acid diarrhoea.
All types of bariatric surgery increase serum total bile acids. The shortened route of enterohepatic circulation speeds up bile acid reabsorption. This leads to earlier and more active bile acid reabsorption.
Other Contributing Factors:
Certain dietary choices and medications can also contribute to bile issues.
High-fat/high-energy intake, processed meat, fish, margarine, and fried potatoes can affect bile production and flow.
Side effects of medications can contribute to bile acid malabsorption. This leads to increased bile acids in the intestines. This can cause bile acid diarrhoea.
Symptoms of Excess Bile

Excess bile in the digestive system causes various uncomfortable symptoms. These symptoms often range from mild to severe. They significantly impact a person’s quality of life. Recognizing these symptoms helps individuals seek proper diagnosis and treatment for bile-related issues.
Gastrointestinal Symptoms:
Many individuals experience distinct gastrointestinal symptoms when they have excess bile. These symptoms often point to bile acid diarrhoea or bile reflux. Common symptoms include frequent diarrhea and watery stool.
Patients also report bloating and stomach cramps. Flatulence is another frequent complaint. A sudden, urgent need for a bowel movement, known as diarrhea urgency, is a hallmark symptom of bile acid diarrhoea. These symptoms arise from bile irritating the colon.
Systemic and Related Indicators:
Beyond the gut, excess bile can manifest through other systemic symptoms. These symptoms often indicate a more widespread issue with bile processing or flow.
Patients may experience changes in bowel frequency and urgency. Nocturnal defecation, or needing to have a bowel movement at night, can occur. Excessive flatulence and abdominal pain are also common symptoms. Incontinence of stool can sometimes develop.
Other systemic symptoms relate to bile accumulation in the body. Dark urine can appear due to excess bilirubin excreted by the kidneys. Pale or clay-colored stools result from a lack of bile reaching the intestine.
Jaundice, a yellowing of the skin and eyes, occurs when bilirubin accumulates in the bloodstream. Itching, known as cholestatic pruritus, happens when bile salts build up in the skin. This itching is often widespread and worsens at night. Fever and chills can signal an infection (cholangitis) in obstructed bile ducts. Bacteria multiply in stagnant bile, causing these symptoms.
When to Seek Medical Advice:
Individuals should seek medical advice if they experience persistent or worsening symptoms of excess bile. Chronic diarrhea, unexplained abdominal pain, or changes in stool color warrant a doctor’s visit.
Jaundice, severe itching, or signs of infection like fever and chills require immediate medical attention. Early diagnosis of these symptoms helps manage bile-related conditions effectively. A healthcare professional can determine the underlying cause of these symptoms and recommend appropriate treatment.
Diagnosing Excess Bile Issues
Initial Assessment and History:
A doctor begins diagnosing excess bile issues with a thorough initial assessment. They ask about a patient’s medical history and symptoms. The doctor focuses on pain characteristics.
They ask about the pain’s location, often in the upper abdomen. They want to know its duration, usually 30 minutes or more. The doctor asks about how often the pain returns. They check its severity. Does it stop daily activities? Does it cause emergency visits? They also ask if bowel movements affect the pain. This correlation is usually weak.
Also The doctor asks if antacids or position changes help the pain. They usually do not improve it much. Associated symptoms are important. These include nausea, vomiting, fever, jaundice, and loss of appetite. The doctor asks if the pain spreads to the back or right shoulder blade.
They also ask if the pain wakes the patient from sleep. They check if pain relievers help. During a physical exam, the doctor looks for specific signs. Murphy’s sign is a sudden stop in breathing due to pain when they press on the right rib. Courvoisier’s sign is an enlarged gallbladder. This often means a blockage. The liver plays a central role in bile production.
Diagnostic Tests for Bile Issues:
Doctors use specific tests to confirm bile issues. The SeHCAT test is the only available diagnostic test for bile acid malabsorption. However, it is expensive and takes time. It also uses radiation.
Four biomarkers help diagnose bile acid malabsorption. These are especially useful for patients with IBS-D. The 75Se-homocholic acid taurine (SeHCAT) test involves taking a radioactive synthetic bile acid. Doctors measure its retention in the abdomen after 7 days. This shows bile acid absorption. Another biomarker is 7α-hydroxy-4-cholesten-3-one (C4). This estimates how fast the liver makes bile acids. Fibroblast growth factor-19 (FGF19) is a hormone.
It reduces bile acid synthesis. The 48-hour fecal bile acid (48FBA) test checks the amount of bile acid leaving the colon. The SeHCAT test shows good accuracy. It has an average sensitivity of 87.3% and specificity of 93.2% for bile acid malabsorption. These values change with the chosen cut-off. For example, an 8% retention cut-off gives 67% sensitivity and 97% specificity.
A 15% retention cut-off gives 100% sensitivity and 91% specificity. A 5% retention cut-off provides 86% sensitivity and 100% specificity. These tests help measure bile acid levels. The liver’s health impacts these levels.
Differentiating from Other Conditions:
It is important to tell the difference between excess bile symptoms and other conditions. Irritable bowel syndrome (IBS) shares some symptoms. These include diarrhea, bloating, tiredness, abdominal pain, and excessive gas. However, bile acid diarrhea has distinct features.
People with bile acid diarrhea have faster stool movement through their large intestines. Their gut microbiomes are less diverse. They have different bacterial compositions. They also show more active genes. These genes are involved in inflammation and gut wall permeability.
These differences help doctors distinguish bile acid diarrhea from IBS. Doctors also differentiate from cholestasis. Cholestasis means reduced bile flow from the liver. This can cause jaundice and itching. It can also lead to liver damage. The liver’s function is key in both conditions. Cholestasis involves a blockage or reduced flow. Excess bile production often involves malabsorption or reflux. The liver’s role in processing bile is crucial for both cholestasis and other bile-related issues.
Relief and Management Strategies
Managing excess bile production involves various approaches. These include medical interventions, dietary changes, and lifestyle adjustments. Patients can find significant relief by combining these strategies.
Medical Treatments and Medications:
Doctors often prescribe specific medications to manage excess bile. These treatments aim to reduce bile acid levels or mitigate their effects.
Bile Acid Sequestrants (BAS): These medications bind to bile acids in the intestine. This prevents their reabsorption and increases their excretion. Cholestyramine is a well-known bile acid sequestrant. It helps patients with intestinal resections of less than 1 meter who experience bile acid diarrhoea. Colesevelam is another option. It offers benefits similar to cholestyramine. However, colesevelam has improved palatability and fewer adverse effects. The effective dose of colesevelam for bile salt malabsorption varies. It ranges between two and six tablets per day in observed cases. An optimal dose is not yet clearly established.
GLP-1 Agonists: Liraglutide, a GLP-1 agonist, has shown effectiveness in some patients. It can lead to complete symptom remission in severe bile acid malabsorption (BAM).
FXR Agonists: Obeticholic acid is a selective FXR agonist. Doctors typically use it for primary biliary cirrhosis. It has also helped a patient with severe BAM and Crohn’s disease when other treatments failed. This medication helps regulate bile acids.
Dietary and Lifestyle Adjustments:
Dietary and lifestyle changes play a crucial role in managing excess bile. These adjustments can reduce symptoms and improve overall digestive health.
Fat Intake Management: Limiting fatty foods helps. High-fat foods can relax the lower esophageal sphincter. They also slow stomach emptying. This can worsen bile reflux. Patients should avoid very high-fat, greasy, or spicy foods. Examples include deep-fried samosas, rich curries, and buttery dishes. These foods temporarily reduce bile acid secretion. Keeping total fat intake under 40 grams per day is often recommended. This means choosing lean proteins and steamed or grilled foods over fried options. Easily digestible fats are better choices. These include avocado, small portions of nuts and seeds, and fatty fish like salmon or mackerel.
Soluble Fiber: Incorporating soluble fiber into the diet is beneficial. Soluble fiber turns to gel during digestion. It helps absorb cholesterol and bile. It then carries them out of the body. Good sources include fruits, vegetables, grains like oatmeal, nuts and seeds, and legumes such as lentils and beans.
Meal Timing and Size: Eating smaller meals more frequently reduces pressure on the lower esophageal sphincter. This can help with bile reflux. Staying upright for two to three hours after a meal allows for proper stomach emptying.
Foods to Avoid for Reflux: Patients should limit or avoid alcohol. Alcohol can relax the lower esophageal sphincter and irritate the esophagus. They should also avoid foods and drinks that increase stomach acid production. These include caffeinated and carbonated beverages, citrus fruits, chocolate, vinegar-based dressings, onions, mint, tomato-based foods, and spicy foods.
Specific Dietary Recommendations: For bile reflux, some suggest cold, wet, or cold and wet foods. These include cucurbit, baked lentil, oat bread, fresh cheese, lettuce, tamarind, coriander, sumac, fresh fish, vinegar, and berberis. Breakfast options might include Sangak bread or oat bread with rose jam. Lunch suggestions feature boiled chicken and baked vegetables. Dinner should be a simple meal, like bread, cucumber, and doogh, rather than meat or legumes.
Individual Triggers: Patients should identify and avoid foods that trigger their individual BAM symptoms. These vary from person to person. Common triggers include spices, dairy, garlic, and gluten.
Combining Strategies: Combining medication with lifestyle adjustments leads to the most significant improvement. This helps manage conditions related to excess bile production.
Complementary Approaches:
Some complementary therapies show promise in managing bile-related digestive issues.
Acupuncture: Acupuncture can significantly reduce esophageal acid and bile reflux. It also improves GERD-related symptoms.
Dietary Considerations:
Resistant starch and fiber: These may help reduce secondary bile acids. They bind to them and increase elimination. Patients can find them in lentils, peas, beans, cooked/cooled rice, whole grains, and firm/green bananas.
Fermentable fiber and plant foods: These support beneficial gut bacteria. They lead to short-chain fatty acid production. This can lower pH and inhibit enzymes that deconjugate bile salts.
Reduced dietary fat intake: This can improve symptoms of bile acid diarrhoea. Fewer bile acids are released for digestion.
Medium-chain triglyceride (MCT) oils: These do not require bile acids for digestion. Patients may tolerate them better.
Supplements and Herbs:
Guggul: This may regulate bile acid transport. It also possesses anti-inflammatory properties.
Probiotics (Lactobacillus genera): These may reduce the amount of bile acids reaching the large bowel. This potentially lessens bile acid diarrhoea severity.
Digestive enzymes: These can aid in digesting proteins, carbohydrates, and fats. They reduce the burden on the digestive tract for those with insufficiency.
Artichoke leaf extract: Studies show this extract significantly increases bile secretion. It also aids in cholesterol regulation by increasing the excretion of bile acids.
Curcumin: In vitro and mice studies indicate curcumin activates FXR. This helps regulate bile acids and mitigate cholestasis. Curcumin also prevents gallstones.
Fenugreek: Rat studies show fenugreek aids in the excretion of bile acids. It has a dose-dependent impact on total bile acid levels in feces. This effect also reduces lipid accumulation in the liver.
Silymarin (Milk Thistle): In vitro studies reveal silymarin activates FXR. This regulates bile action homeostasis. A follow-up mice study showed silymarin decreased the number of bile acids in feces and the liver.
Traditional Chinese Medicine (TCM): A study on TCM demonstrated that the herbal combination of rhubarb and gardenia provided protective effects to the liver in rats with induced cholestasis. The synergy of the two herbs enhanced the effect compared to single herbs. This suggests potential for preventing liver damage.
Excess bile production presents varied causes, including malabsorption and reflux, and diverse symptoms. These issues significantly impact digestive health. Individuals find effective relief and management through accurate diagnosis and a tailored treatment plan. Always consult healthcare professionals for personalized guidance. Do not self-diagnose or self-treat. Informed management of bile-related conditions improves quality of life.