Experiencing hip pain can be incredibly disruptive. This discomfort often impacts your daily life. The exact location of your pain holds a significant clue to its underlying cause. Hip pain can stem from various issues, like arthritis, tendinitis, or labral tears. This hip pain location chart helps you quickly identify potential sources of your hip discomfort.
You can better understand the pain in your hips by pinpointing where it hurts most.
Key Takeaways
The exact spot of your hip pain helps find its cause. Different areas of pain mean different problems.
This chart helps you understand your hip pain. It shows common pain areas and possible reasons.
Pain in the front of your hip can mean hip flexor issues or a labral tear. It can also be hip arthritis or FAI.
Pain on the side of your hip often comes from trochanteric bursitis or gluteal tendinopathy. IT band syndrome can also cause this pain.
See a doctor if your hip pain is severe or sudden. Also, get help if you cannot walk or have a fever.
Understanding Hip Pain Location
Why Location Matters
When you experience hip pain, its exact location provides important clues. Your hip is a complex joint. Many different structures can cause pain. Knowing where your pain is helps narrow down the possibilities. For example, pain in the front of your hip suggests different issues than pain on the side.
Pain in the back of your hip also points to unique problems. This guide helps you understand these differences. You can then talk more clearly with your doctor about your hip. The precise location of your pain is often the first step in finding the right diagnosis.
It helps your doctor understand what might be causing your hip discomfort. Different conditions affect different parts of the hip. Pinpointing the pain’s origin is crucial for effective treatment. This initial understanding of your hip pain is very powerful.
How This Chart Guides You
This hip pain location chart acts like a map for your body. You can use it to identify the specific area of your discomfort. Think of it as a hip pain diagram. It shows you common areas where pain occurs.
Then, it links those areas to possible causes. This chart does not give a diagnosis. It helps you understand your symptoms better. You will learn about different types of hip pain. This knowledge helps you describe your pain accurately. You can then discuss your hip issues with a healthcare professional. This helps them find the right treatment for your hip pain.
Understanding the location of your pain is your first step. This hip pain location chart empowers you with knowledge about your hip. You can use this tool to prepare for your doctor’s visit. This makes your conversation more productive. It helps you become an active participant in your own care.
Front Hip Pain Causes

Pain in the front of your hip often points to specific issues. This area includes your hip joint, muscles, and tendons. Understanding these common causes helps you identify the source of your discomfort. Pain radiating down your thigh to your knee from this region often indicates a hip problem.
Hip Flexor Issues
Your hip flexors are a group of muscles. They help you lift your knee towards your chest. These muscles connect your upper leg to your pelvis. The iliacus muscle is one important hip flexor. Prolonged sitting and poor posture can often make hip flexor issues worse. When these muscles get strained or tight, you feel pain in the front of your hip.
You might notice several symptoms if you have hip flexor issues:
You feel pain at the front of your hip, where your thigh meets your pelvis. This pain can range from a mild ache to sharp, stabbing pain.
Your hips feel tight or weak, especially after sitting for a long time.
You experience sharp pain in the front of your hip during movement or even at rest. This often happens with pulled hip flexors.
You might see swelling or bruising if you have torn hip flexors.
Moving your leg or walking becomes difficult due to limited range of motion.
Your affected leg feels weaker or unstable.
The front of your hip feels tender or sensitive when you touch it.
You might feel a pulling sensation in the front of your hip.
A dull ache can occur in your lower back.
Your hip area feels stiff.
Everyday activities like walking or standing straight cause discomfort.
Tightness increases after prolonged sitting, during exercise, or when you perform hip flexion movements like climbing stairs or squatting.
Diagnosing a hip flexor strain involves reviewing your symptoms and medical history. Your doctor will conduct a physical examination.
They will check your affected hip for pain, swelling, and inflammation. Doctors may also order imaging tests. These tests include X-rays, CT scans, or MRI scans. Specific tests help doctors understand the problem:
Active range of motion testing
Passive range of motion testing
Thomas test
Magnetic Resonance Imaging (MRI)
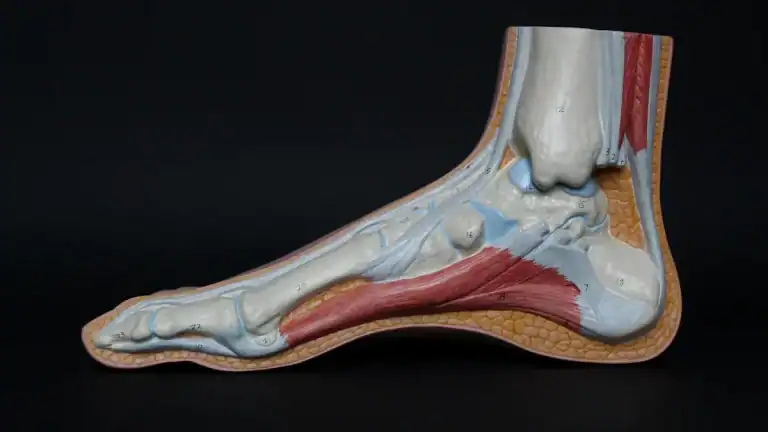
Labral Tears
Your hip joint has a ring of cartilage called the labrum. This labrum lines the rim of your hip socket. It helps cushion the joint and keeps the ball of your thigh bone in place. A labral tear happens when this cartilage gets damaged. This can cause significant hip pain.
Several factors can lead to a hip labral tear:
Trauma: A significant injury during contact sports can cause a tear. Hip subluxation (partial dislocation) or dislocation can also lead to tears.
Femoroacetabular Impingement (FAI): This condition involves abnormal bone shapes in your hip. It can pinch the labrum.
Capsular Laxity or Hip Hypermobility: If your hip joint is too loose, it can put stress on the labrum.
Dysplasia: This means your hip socket is not shaped correctly.
Degeneration: Over time, the labrum can wear down.
Hip Flexion Contracture: Muscle imbalances can increase weight on the front of your hip socket and labrum.
Labral tears are common, especially in athletes. The prevalence of acetabular labral tears in athletes participating in noncontact sports ranges from 22% to 100%. Interestingly, 50-60% of labral tears in competitive athletes may not cause any symptoms.
Hip Osteoarthritis
Hip osteoarthritis is a common condition. It involves the breakdown of cartilage in your hip joint.
Cartilage provides a smooth surface for your bones to glide. When it wears away, bones rub against each other. This causes pain and stiffness. This condition often leads to pain in the front of your hip.
You might notice these early signs and symptoms of hip osteoarthritis:
feel pain and stiffness when your hip joint moves.
hip has a limited range of motion.
You find it difficult to bend at your waist or you walk with a limp.
You feel a grinding or locking sensation when you move your hip.
You hear a crackling or clicking sound (crepitus) when your hip moves.
You might feel referred pain in areas around your hip joint. This includes your groin, thigh, buttocks, or knee.
Your hip may hurt during or after movement.
Stiffness is most noticeable when you wake up or after you have been inactive.
You lose flexibility, making it hard to move your hip through its full range of motion.
You feel or hear a grating sensation when you stand, walk, or climb stairs.
Many factors increase your risk of developing hip osteoarthritis:
Older age: Your risk increases as you get older.
Obesity: Extra weight puts more stress on your hip joints.
Genetics: Your family history plays a role.
Repetitive stress and mechanical overload: Certain jobs or high-impact sports can increase risk. Examples include farming, construction work, football, hockey, wrestling, weight-lifting, and long-distance running.
Hip abnormalities: Conditions like acetabular dysplasia or femoroacetabular impingement can lead to osteoarthritis.
Trauma: A hip dislocation or fracture can cause problems years later.
Femoroacetabular Impingement
Femoroacetabular impingement (FAI) happens when the bones in your hip joint rub or catch against each other. This usually occurs because of extra bone growth, called a bone spur. This spur can be on your thigh bone or inside your hip socket. This condition often causes pain in the front of your hip.
FAI commonly appears in two forms:
Cam Impingement: Your femoral head (the ball of your thigh bone) is not perfectly round. This causes abnormal contact with your hip socket during movement.
Pincer Impingement: Your hip socket (acetabulum) has too much coverage over the femoral head. This often happens along the front-top rim.
Both Cam and Pincer forms can happen together. These bone variations pinch the labral cartilage between the socket rim and the thigh bone.
Several factors contribute to FAI:
Congenital hip deformities: These are hip abnormalities present at birth.
Irregular bone growth: This can happen during childhood.
Genetic predisposition: Family history can increase your risk.
Pelvic or spinal misalignment.
Intense sporting activities: Participating in these during adolescence, when bones are still developing, can be a factor.
Other hip disorders: Conditions like Perthes disease and slipped capital femoral epiphysis link to FAI.
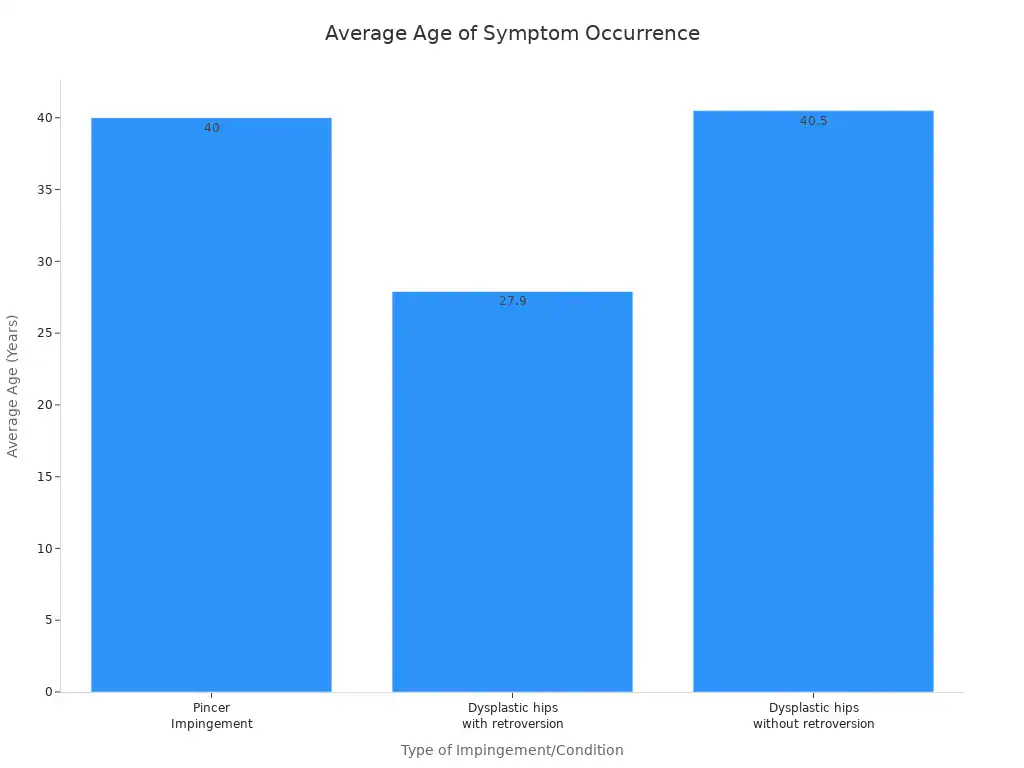
FAI is typically diagnosed in adolescents and young adults. One study found the average age of FAI patients was 35 years. The age of symptom occurrence can vary by type:
Type of Impingement/Condition | Average Age of Symptom Occurrence |
|---|---|
Pincer Impingement | 40 years |
Dysplastic hips with retroversion | 27.9 years |
Dysplastic hips without retroversion | 40.5 years |
Side Hip Pain Causes
Pain on the outer aspect of your hip often signals specific conditions. This area includes important muscles, tendons, and fluid-filled sacs called bursae. Understanding these common causes helps you identify the source of your discomfort.
Trochanteric Bursitis
Trochanteric bursitis involves inflammation of the bursa located on the outside of your hip. This bursa cushions your hip bone. When it becomes inflamed, you feel pain. This condition causes chronic, intermittent aching pain over the side of your hip.
You might experience several symptoms with trochanteric bursitis:
You feel pain at the point of your hip. This pain often extends to the outside of your thigh.
Initially, the pain is sharp and intense. Later, it becomes a dull ache that spreads across a larger hip area.
The pain typically worsens at night, especially when you lie on the affected hip.
You feel more pain upon standing after sitting for a while.
Prolonged walking, climbing stairs, or squatting can increase your discomfort.
Moving your hip joint causes pain.
Lying on the affected side of your body makes the pain worse.
Your hip feels tender.
You might limp.
You notice soreness or swelling in your hip.
The pain may spread down your leg toward your knee.
Transitioning from sitting to standing or climbing stairs becomes challenging.
Conservative treatments often help with trochanteric bursitis. Corticosteroid injections can offer significant relief. Studies show improvement rates of 60-66% at one and five years with these injections. A randomized controlled trial found a 55% recovery rate in the injection group at three months, compared to 34% in the usual care group. At 12 months, both groups reached similar recovery rates of 60-61%.
Gluteal Tendinopathy
Gluteal tendinopathy involves damage or degeneration of the tendons of your gluteal muscles. These muscles are in your buttocks and connect to the side of your hip. This condition causes pain on the side of your hip.
Several factors can lead to gluteal tendinopathy:
Too much activity too soon: You might rapidly increase exercise intensity without proper conditioning.
Inactivity: Frequent sitting without changing positions can irritate your tendons.
Acute injury: Falling and landing on your hip can cause damage.
Disorganization of collagen fibers: The structure of your tendons can break down.
Lack of strength and stability: Your hip muscles might not be strong enough.
Hormonal changes: A drop in estrogen levels during menopause can affect tendon health.
Aging: You naturally lose muscle mass and produce less collagen as you age.
Overuse or excessive force: Physical activities can put too much stress on your tendons.
Compression: Acute injuries like falls can compress your tendons.
Weight gain or obesity: Extra weight places more pressure on your hip tendons.
Underuse or inactivity: A sedentary lifestyle can contribute to the problem.
Instability: Wide hips or pelvis can cause instability.
Rehabilitation exercises are crucial for gluteal tendinopathy. You can perform exercises that mimic day-to-day activities:
Bridge: Lie on your back, squeeze your glutes, and lift your hips. You can progress to staggered legs or single-leg bridges. Aim for 3 sets of 20 repetitions.
Sit-to-stand: From a chair, lean forward, stand up, and slowly sit back down. Use your hands for assistance if you need it. You can hold a weight to increase difficulty. Aim for 3 sets of 20 repetitions.
Step-up: Use stairs or sturdy objects. Decrease the height or use your hands for assistance if you need it. Aim for 3 sets of 10 repetitions per leg.
Single-leg balance: Squeeze the glutes of your standing leg. Use your hands for assistance. Build up to 3 sets of 60 seconds.
You can also do gluteus medius specific strengthening exercises:
Band push-out: Place a band above your knees. Lie on your back with a pillow under your knees. Push out into the band for 30-45 seconds.
Standing floor spread: Stand with your heels hip-width apart or wider. Imagine spreading the floor with your feet. Hold for 30-45 seconds.
Side-lying leg lift: Lie on your unaffected side with your bottom hip and knee bent. Rest your top leg on two pillows. Keep your knee straight. Slightly lift your top leg off the pillows. Hold for 30-45 seconds. You can add a band or weight for more challenge.
Advanced exercises include single-leg hip thrusts, split squats, single-leg deadlifts, side planks, and banded side steps.
IT Band Syndrome
Iliotibial band (IT band) syndrome causes pain on the outside of your knee, but it can also cause pain on the side of your hip. Your IT band is a thick band of tissue that runs along the outside of your thigh. It extends from your hip to your shin bone. When this band becomes tight or inflamed, it causes pain.
Certain activities commonly aggravate IT band syndrome:
Running or Cycling: These activities are common triggers. Their repetitive nature affects long-distance athletes especially.
Squats or Lunges: These exercises often cause pain with an IT band injury. This is particularly true when your knee bends between 30 and 90 degrees.
Improper Foam Rolling: Foam rolling can be beneficial. However, incorrect technique or applying it directly to an already sore IT band can make your pain worse.
The role of stretching in treating IT band syndrome is often discussed. Stretching is a common part of ITBS rehabilitation. However, its specific effectiveness and superiority over other treatments are not definitively established. Some studies show non-significant improvements in pain with stretching.
These improvements are comparable to or not better than hip strengthening exercises. While stretching may cause some elongation of the ITB, particularly in the upper part including the TFL muscle, observed improvements in hip range of motion could be due to increased flexibility of the TFL rather than the ITB itself. The benefit of ITB-TFL complex stretching for ITBS treatment and prevention is debated. Some risk factors might resolve, while others could worsen. The main theory for ITBS suggests compression, which stretching does not directly change.
Here are some findings on stretching for ITBS:
Author (Year) | Population | Intervention | Findings |
|---|---|---|---|
Pepper et al., 2021 | Healthy adults (18–50 years) | Stretching (7s submaximal contraction + 15s stretch) | No effects on ITB stiffness, despite increases in hip RoM. |
McKay et al., 2020 | Female distance runners (19–45 years) with unilateral ITBS | Progressive stretching program (30–40s hold, 2–4 times, 3x/week for 8 weeks) | Non-significant improvement in pain; no statistical differences compared to conventional hip rehabilitation or experimental exercises. |
Afshari et al., 2023 | Semi-elite athletes (20–40 years) with ITB shortness | PNF active stretching (3–5 min) | Significant increase in active hip adduction RoM, single-leg hop, lateral hop, and vertical jump, with similar changes across all intervention groups (including FR and combination). |
Kasunich, 2003 | Case report: long-distance runner (38 years) with low-back and sacroiliac pain | Extensive ITB stretching (once/day for 2 weeks, twice/day for 2 weeks) | Patient showed significant improvement only after extensive stretching was included in the treatment plan. |
Back Hip and Buttock Pain Causes

Pain originating from the posterior hip and gluteal region can come from various sources. Understanding these conditions helps you pinpoint the cause of your discomfort.
Piriformis Syndrome
Piriformis syndrome causes pain, tingling, and numbness in your buttocks. This discomfort can also extend down your leg. You might feel a shooting pain that starts at your hip or buttocks and goes down your leg to your foot. This pain often worsens when you stretch your piriformis muscle. You may also experience foot and leg weakness, sometimes leading to foot drop.
This makes it hard to lift your foot while walking. You might also notice changes in sensation in your affected leg. This happens because the sciatic nerve gets pinched. Your pain in the back of your hip often increases after sitting for more than 15 to 20 minutes. You might feel tenderness and a muscle spasm in your piriformis muscle.
Sacroiliac Joint Dysfunction
Sacroiliac (SI) joint dysfunction happens when the joint connecting your sacrum to your pelvis does not move correctly. This causes pain in your lower back and buttocks. Many factors can cause this dysfunction:
Hypermobility: Your ligaments are too loose, causing instability.
Pregnancy: Ligaments stretch for childbirth, adding stress to the joint.
Injury: Falls or accidents can strain or tear SI joint ligaments.
Degenerative joint diseases: Arthritis can cause cartilage to wear down.
Spinal fusion: This can put extra stress on your SI joint.
Uneven leg length: This creates uneven movement in your pelvis.
Doctors use specific tests to diagnose SI joint dysfunction. These are called provocative tests. They involve manipulating your hip joints. Examples include the FABER test, Thigh Thrust test, and Gaenslen test. If three or more of these tests reproduce your pain, doctors can reasonably conclude you have SI joint dysfunction.
Hamstring Tendinopathy
Hamstring tendinopathy involves damage to the tendons of your hamstring muscles. These muscles run down the back of your thigh. This condition causes pain in the back of your hip and thigh.
The recovery time for hamstring tendinopathy depends on how severe your injury is. Lower-grade tears can heal quickly, sometimes in less than a week. However, more severe injuries can take several months to heal. Most people recover well and return to their activities. Some minimal pain might last for a few extra weeks.
Sciatica and Referred Pain
Sciatica occurs when your sciatic nerve gets irritated or compressed. This nerve runs from your lower back, through your buttocks, and down each leg. It causes pain that radiates along its path. Common causes include:
Herniated disks
Spinal stenosis (narrowing of the spinal canal)
Piriformis syndrome
Pregnancy
Degenerative disk disease
You can manage sciatica with non-surgical treatments. Physical therapy helps strengthen your core and stretch tight muscles. Hot and cold therapy can reduce inflammation and muscle tension. Medications like NSAIDs can offer short-term pain relief. Epidural steroid injections can also reduce inflammation around the nerve roots.
Groin Pain Causes
Pain in your groin can often link to issues with your hip. This section details conditions that specifically cause groin pain.
Adductor Strain
An adductor strain happens when you injure the muscles on the inside of your thigh. These muscles help you bring your legs together. This injury often causes sudden groin pain.
Athletes commonly get adductor strains. Several actions can cause this:
Direct blunt trauma: A direct hit to your inner thigh can cause injury.
Forceful contraction: This is a common cause. It happens during actions like:
Changing direction quickly
Kicking a ball
Reaching or stretching too far
Jumping
Strong muscle contractions
Microtrauma by repetitive injury: Repeated small injuries can lead to chronic groin pain.
If you experience an adductor strain, follow a recovery protocol.
Stop all exercise: Rest your leg and keep it elevated. You can move gently after about 48 hours.
Apply RICE: Use Rest, Ice, Compression, and Elevation to reduce pain and swelling. Apply ice for 10-15 minutes every few hours.
Treat quickly: Address the strain within 24 to 48 hours. This helps reduce bleeding and inflammation.
See a Physiotherapist: A physiotherapist helps you regain full strength in your adductor muscles.
Sports Hernia
A sports hernia causes chronic groin pain. Doctors also call it athletic pubalgia. This condition involves soft tissue injuries in your groin area. It often happens during high-intensity sports. The term “sports hernia” is a bit misleading. Most cases do not involve tissue pushing through a hole.
Doctors use specific criteria to diagnose a sports hernia:
Criterion | Description |
|---|---|
History | You participate in high-intensity athletic activity. |
Symptoms | You have typical hernia symptoms, but no physical evidence on examination. |
Physical Exam | You feel pain when you push your legs together against resistance. |
Bulge | No bulge appears when you strain. |
MRI and ultrasound can also help diagnose this condition. After surgery for a sports hernia, many athletes return to their sport. About 80% of athletes return to their pre-injury activity level. You can expect good hip function and low pain long-term.
Avascular Necrosis
Avascular necrosis (AVN) happens when your hip bone does not get enough blood. This lack of blood flow causes bone tissue to die. This can lead to severe hip pain.
Several factors increase your risk for AVN:
Injury or Trauma: Hip fractures or dislocations can damage blood vessels.
Long-Term Corticosteroid Use: High doses of steroids can reduce blood flow.
Heavy Alcohol Use: This can cause fat buildup in blood vessels.
Medical Conditions: Sickle cell anemia or lupus can affect blood flow.
Cancer Treatments: Radiation and chemotherapy can weaken bones.
Early diagnosis is important for AVN. Doctors look at your history and do a physical exam. They consider risk factors like steroid use or alcohol abuse. MRI is especially useful and sensitive for early detection. It can show signs of AVN even before you feel symptoms.
When to Seek Help for Hip Pain
Red Flag Symptoms
You need to know when your hip pain requires immediate medical attention. Certain symptoms are red flags. Do not ignore these signs.
You experience sudden, severe pain. This pain might come on without warning.
You cannot bear weight on your hip. Walking becomes impossible or extremely difficult.
Your hip joint looks deformed. You might see an unusual shape or position.
You have intense pain, swelling, or bruising around your hip. These signs can indicate a serious injury.
You develop a fever, chills, or other signs of infection. This could mean an infected joint.
Your pain worsens at night or wakes you from sleep. This can be a sign of inflammation or other issues.
You have numbness or tingling in your leg or foot. This suggests nerve involvement.
You experience new bowel or bladder changes. This is a critical sign requiring urgent care. These symptoms suggest a serious problem. Seek professional help right away.
Importance of Diagnosis
A proper diagnosis identifies the exact cause of your discomfort. This guide, like a hip pain location chart, helps you understand potential issues. However, it does not replace a doctor’s expertise.
A medical professional can perform a thorough examination. They might order imaging tests, such as X-rays or MRI scans. These tests help confirm the source of your hip pain. An accurate diagnosis leads to effective treatment. It prevents further complications. Do not self-diagnose serious conditions. You need a professional assessment for your hip.
Preparing for Your Visit
Prepare for your doctor’s appointment. This helps your doctor understand your symptoms better.
Describe your pain location precisely. Use this hip pain diagram as a reference. Point to the exact spot where you feel the pain.
Note when your pain started. Was it sudden or gradual?
Explain what makes your pain better or worse. Does rest help? Does activity worsen it?
List any other symptoms you have. Include any associated numbness, tingling, or weakness.
Bring a list of all your current medications.
Mention any recent injuries or changes in your activity level. This detailed information helps your doctor make an accurate diagnosis. You get the right treatment plan for your hip.
While this guide offers valuable insights, it is not a substitute for professional medical diagnosis. Use this information to have more informed conversations with your healthcare providers. They can give you the right answers.