Leg pain is a common experience. You might feel minor aches or debilitating discomfort. This leg pain often comes from wear and tear, overuse, or injuries. Understanding the potential causes of your leg pain is important for self-care. It also helps you know when to seek professional help. This Leg Pain Identifier Chart is a practical tool.
It helps you systematically analyze your symptoms. You can look at the pain’s location and characteristics. This bridges the gap between your symptoms and a potential diagnosis. Common causes of leg pain include muscle cramps, strains, shin splints, and issues like Peripheral Artery Disease.
This article aims to empower you with knowledge for understanding leg pain. It will guide you on appropriate next steps for diagnosing leg pain.
Key Takeaways
Leg pain can come from many places, like muscles, nerves, or blood vessels. Knowing where your pain is helps you understand why it hurts.
Some leg pain needs a doctor right away. Look for sudden, bad pain, swelling, warmth, or trouble breathing. These are serious signs.
Conditions like muscle strains often get better with rest. Other problems, like blood clots or nerve issues, need quick medical care.
Leg Pain Above Knee
When you experience leg pain above the knee, the exact location and type of discomfort can tell you a lot. This area includes your front, outer, and back thigh, as well as your hip and groin. Understanding these differences helps you pinpoint the potential cause of your leg pain.
Front Thigh Pain
Pain in the front of your thigh often points to issues with your quadriceps muscles or certain nerves. You might feel a sharp, sudden pain or a dull, persistent ache.
Quadriceps Strain: This happens when you injure the large muscles at the front of your thigh. These muscles help you straighten your knee. Overuse or sudden trauma can cause this. You might feel pain and weakness when you try to straighten your knee. Stairs or squatting can also hurt.
Quadriceps Tendon Injury: This is similar to a quadriceps strain but affects the tendon just above your kneecap. The pain is more focused at the top of your kneecap. Severe cases can make it hard or impossible to straighten your knee.
Hip Flexor Strain (Iliopsoas): These muscles are at the front of your hip. They help you lift your leg. Inactivity, overuse, or sudden injury can lead to pain and stiffness in your front thigh and groin.
Iliopsoas Bursitis: A bursa is a small fluid-filled sac that reduces friction. If the bursa behind your iliopsoas muscle gets inflamed, you feel a deep ache in your hip and groin. Lifting your leg can make this pain worse. Repetitive actions like running or kicking often cause it.
Nerve Injuries: Nerves from your lower back can cause symptoms in your front thighs. You might feel burning, pins and needles, numbness, or changes in sensation or temperature.
Meralgia Paresthetica: This condition causes pain, aching, burning, or numbness in your thigh. It happens when the lateral femoral cutaneous nerve (LFCN) gets compressed.
It is important to distinguish between different conditions. For example, a quadriceps strain feels like localized pain in the muscle. You will feel pain when you resist knee extension. However, a femoral stress fracture, which is a tiny crack in your thigh bone, presents differently.
Symptom | Quadriceps Strain | Femoral Stress Fracture |
|---|---|---|
Tenderness | Localized in the quadriceps muscle | Vague, poorly localized discomfort in thigh/knee |
Resisted Testing | Pain with resisted knee extension | Not typically painful with resisted quads |
Limping | Often no limp | Often present |
Single Hop Test | Often no pain with a single hop | Painful or unable to perform |
Commonality in Runners | Rare in endurance runners | More common in endurance runners |
Femoral shaft stress fractures often cause vague discomfort around your thigh or knee. You might mistake these symptoms for a quadriceps strain. Quadriceps strains are rare in endurance runners, but femoral stress fractures are more common in this group.
Outer Thigh Pain
Pain on the outer side of your thigh can stem from nerve issues, muscle problems, or even referred pain from your hip.
Meralgia Paresthetica: This condition can cause tingling, numbness, and a burning pain in your outer thigh. It typically affects one side of your body. Pressure on the lateral femoral cutaneous nerve causes it.
Sciatica: This nerve pain starts in your lower back or hip. It can spread to your thigh. A compressed sciatic nerve, perhaps from a herniated disk, causes it.
Soft Tissue Injuries: Injuries to your muscles, ligaments, and tendons can cause aching pain and sometimes swelling. These often result from physical activity.
Joint Pain: Pain in your hip joint, often from conditions like osteoarthritis, can radiate to your thigh. It can also cause muscle tension.
Pregnancy: The pressure from pregnancy can cause aches, including pelvic girdle pain. This pain can spread to your thighs.
Broken Bones: A fractured thigh or hip bone, usually from a fall or injury, causes intense pain. You will have difficulty walking.
Back Thigh Pain
Pain in the back of your thigh often involves your hamstring muscles or nerves originating from your lower back.
Hamstring Strain or Tear: This is a common injury, especially in athletes. You might feel a sudden “pull” or snap during activities like running or kicking. The pain is isolated to the back of your thigh or upper buttock. The area might feel tender, bruised, or swollen. Stretching your hamstring or bending your knee causes discomfort.
Hamstring Tendinopathy: This is an overuse injury affecting the hamstring tendons.
Sciatica: This nerve pain can travel down the back of your leg. It often starts in your lower back or buttock. You might feel tingling, numbness, or weakness in your leg or foot. Sitting for long periods or bending forward can worsen the pain. The pain is sharp, shooting, or feels like an electric shock.
Piriformis Syndrome: The piriformis muscle is deep in your buttock. If it spasms or compresses the sciatic nerve, you can feel pain in your buttock and down the back of your thigh.
Spinal Nerve Compression: Conditions like herniated disks, bone spurs, or spinal stenosis in your lower back can compress nerves. This causes referred leg pain down your thigh.
Peripheral Arterial Disease (PAD): This condition affects blood flow. It can cause cramping or fatigue in your leg muscles during exercise. This pain often eases with rest.
Bursitis (Trochanteric bursitis/Greater Trochanteric Pain Syndrome – GTPS): Inflammation of the bursa near your hip bone can cause pain that radiates down your outer or back thigh.
Deep Vein Thrombosis (DVT): This is a serious condition where a blood clot forms in a deep vein. It can cause pain, swelling, warmth, and redness in your leg. Seek immediate medical attention if you suspect DVT.
It is crucial to tell the difference between a hamstring strain and sciatica.
Stretch Test: If stretching your hamstring causes sharp, localized muscle pain, it is likely a strain. If it sends shooting pain down your leg or into your foot, it could be sciatica.
Sit Test: Sciatic pain often worsens with prolonged sitting. A hamstring strain might feel stiff at rest but will not trigger nerve-like pain.
Massage Response: Gentle massage may help with hamstring muscle soreness. Nerve pain from sciatica typically will not improve and might even worsen with pressure.
Pain Location: Hamstring pain is usually from the base of your buttock to the middle of your thigh. It does not radiate below the knee. Sciatica can extend from your lower back all the way to your toes.
Type of Pain: Sciatica involves shooting pain, pins and needles, or hot/cold sensations. Hamstring pain is more of a localized tightness.
Feature | Sciatica | Hamstring Pain |
|---|---|---|
Pain Location | Lower back, buttock, leg (often below knee) | Back of thigh or upper buttock (stays above knee) |
Pain Type | Sharp, burning, electric, with tingling or numbness | Dull ache, tightness, cramping sensation |
Onset | Gradual or sudden; triggered by sitting/bending | Often sudden during sport or overuse |
Triggers | Sitting, lifting, bending, coughing | Running, jumping, stretching, overuse |
Range of Motion | Limited by nerve irritation, especially bending | Limited by muscle stretch or contraction |
Hip and Groin Pain
Pain in your hip and groin area can be complex. It often involves the hip joint itself, surrounding muscles, or even referred pain from your spine. These are common pelvic and hip problems.
Osteoarthritis (OA) of the Hip: This is a degenerative joint condition. You might feel pain deep in your hip, especially in the front. It often causes stiffness, particularly after resting or in the morning. Your first few steps after sitting for a while can be painful.
Femoroacetabular Impingement (FAI): This happens when extra bone grows along one or both of the bones that form your hip joint. This extra bone causes the bones to rub against each other. It can cause pain and limit your hip movement.
Muscle Strains:
Adductor Injury (Groin Strain): This affects the muscles on the inside of your thigh. It often causes sudden pain during activity.
Hip Flexor Strain: As mentioned, this can cause pain in the front of your hip and groin.
Gluteus Tendinopathy: This affects the tendons of your gluteal muscles. It causes pain on the side of your hip that can radiate down your thigh.
Trochanteric Bursitis: Inflammation of the bursa on the outside of your hip. It causes pain on the outer hip that can spread down your thigh.
Hernia: A hernia in the groin can cause pain, especially when you lift, cough, or strain.
Referred Pain from the Lower Spine: Issues like a herniated disk or spinal stenosis can cause leg pain that you feel in your hip or groin.
Acute Onset Conditions: These include muscle strains, contusions (like a hip pointer), hip dislocations, labral tears, and proximal femur fractures. These usually result from a specific injury.
Insidious Onset Conditions: These develop over time. They include sports hernias, osteitis pubis, snapping hip syndrome, and stress syndrome.
Avascular Necrosis: This happens when blood flow to the bone tissue is interrupted, causing bone death. It can lead to severe hip pain.
Endometriosis or Ovarian Cysts: In women, these conditions can sometimes cause pain that radiates to the hip or groin.
Joint Infection in the Hip: This is a serious condition causing severe pain, swelling, and fever.
Psoriatic Arthritis or Rheumatoid Arthritis: These inflammatory conditions can affect the hip joint, causing pain and stiffness.
It is helpful to differentiate between a hip flexor strain and hip osteoarthritis.
Symptom Category | Hip Flexor Strain | Hip Osteoarthritis |
|---|---|---|
Pain Location | Groin area, outside of the hip, occasionally front of the hip (superficial) | Front of the hip (deeper, near the joint) |
Aggravating Activities | Aggressive activities, twisting leg, crossing legs | First few steps in the morning, after sitting for a while, internal rotation of the foot |
Associated Sensations | Discomfort during specific leg movements, stretching sensation | Stiffness, takes time to warm up and free up |
Underlying Cause | Muscle imbalance (overactive hip flexors due to weak glutes/abs) | Degenerative joint changes |
Understanding the specific characteristics of your leg pain above the knee is the first step. This helps you identify the potential cause and decide on the next steps for effective treatment.
Knee Pain Location
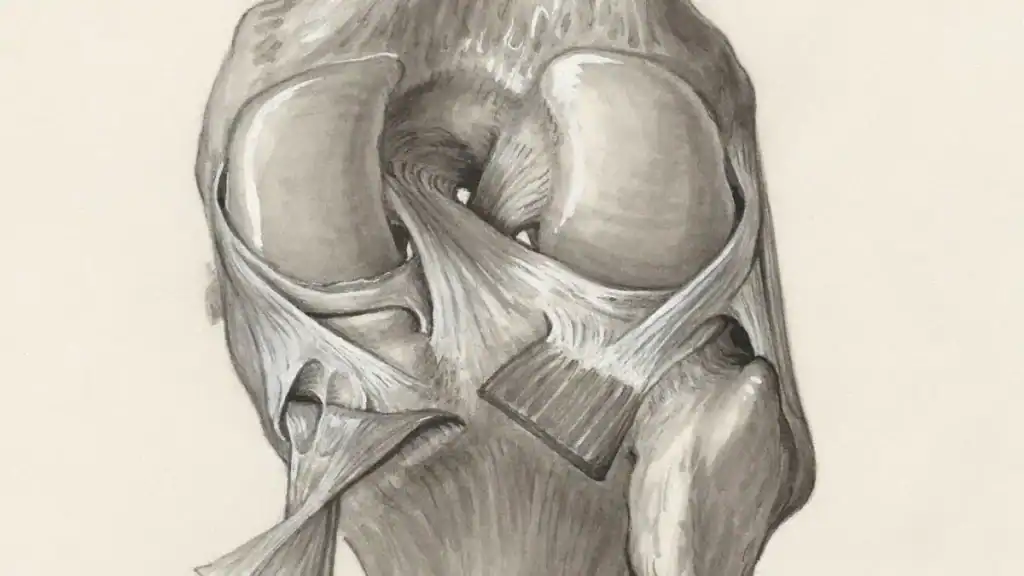
Knee pain is a very common complaint. You can feel this knee pain in many different spots. The exact location of your knee pain helps you understand its cause. Let’s explore where you might feel knee pain and what it could mean.
Pain Above Kneecap
When you feel knee pain above your kneecap, several conditions might be the cause. This type of leg pain often involves the structures around the top of your knee.
Patellofemoral Syndrome: Your kneecap does not move smoothly in its groove. This causes knee pain above the knee. Athletes like basketball players, runners, and cyclists often experience this.
Meniscal Tears: The cartilage cushioning your knee joint can tear. This causes knee pain above the knee. Athletes and older people commonly get these tears.
Osteoarthritis: This arthritis affects your knee joint. It leads to knee pain and stiffness above the knee. People over 50 often experience this.
Knee Ligament Sprains (ACL): A sprain or tear of your anterior cruciate ligament (ACL) can cause knee pain above the knee. Sports like soccer, basketball, or football often cause these injuries.
Iliotibial Band Friction Syndrome (ITB): Your ITB rubs over the side of your thigh bone. This causes inflammation and knee pain above the knee. Runners and cyclists often get this from repetitive movements.
Patellar Tendonitis: This is inflammation of the tendon connecting your kneecap to your thighbone. Overuse of your knee typically causes it.
Patellar Bursitis: The bursa in front of your kneecap can become inflamed. A forceful impact or too much kneeling often causes this. You will feel swelling and knee pain.
Patellofemoral Disorders: These conditions affect where your kneecap meets your thigh bone. They can lead to knee pain in this area.
Pain Below Kneecap
Pain below your kneecap often points to issues with the patellar tendon or growth plates. This leg pain can feel sharp or dull.
Patellar Tendonitis (Jumper’s Knee): This is inflammation of the tendon just below your kneecap. Repetitive jumping or running often causes it. You feel pain when you jump, run, or climb stairs.
Osgood-Schlatter Disease: This condition affects growing adolescents. It causes pain and swelling below the kneecap. It happens when the patellar tendon pulls on the shinbone’s growth plate.
Infrapatellar Bursitis: The bursa located below your kneecap can become inflamed. Direct trauma or overuse can cause this. You might notice swelling and tenderness.
Shin Splints (Medial Tibial Stress Syndrome): While often felt in the shin, severe cases can cause referred leg pain that feels like it’s just below the kneecap. This happens from overuse, especially in runners.
Inner Knee Pain
Inner knee pain occurs on the side of your knee closest to your other leg. Many different conditions can cause this type of leg pain.
Osteoarthritis (OA): This degenerative disease breaks down cartilage. It often affects the inner part of your knee. You might feel stiffness and knee pain.
Rheumatoid Arthritis (RA): This autoimmune disease causes joint pain, swelling, and stiffness. It can affect your inner knee.
Medial Collateral Ligament (MCL) Injury: This ligament is on the inside of your knee. It can overstretch or tear. This causes knee pain and instability.
Medial Meniscus Injury: Damage to the cartilage cushion between your bones can cause inner knee pain. You might feel clicking or locking.
Pes Anserine Bursitis: The bursa on the lower inner part of your knee can get inflamed. Overuse or irritation often causes this.
Medial Plica Irritation: Small folds in your joint lining can thicken from overuse. This causes inner knee pain.
Other Injuries: A direct blow can cause a knee contusion. Avascular necrosis or saphenous nerve irritation can also cause inner knee pain.
Outer Knee Pain
Pain on the outer side of your knee can also be quite bothersome. This leg pain often comes from overuse or specific injuries.
Iliotibial Band Friction Syndrome (ITBS): Your IT band runs along the outside of your thigh. It can rub against your outer knee bone. This causes inflammation and knee pain. Runners and cyclists often experience this.
Lateral Meniscus Injury: Damage to the cartilage on the outer side of your knee can cause knee pain. You might feel a catching sensation.
Lateral Collateral Ligament (LCL) Injury: This ligament is on the outside of your knee. A direct blow to the inside of your knee can injure it. This causes knee pain and instability.
Biceps Femoris Tendinopathy: The tendon of your biceps femoris muscle (part of your hamstring) attaches to the outer knee. Overuse can inflame it, causing knee pain.
Behind Knee Pain
Pain behind your knee can be concerning. This type of leg pain can range from mild discomfort to severe issues. Finding the cause is important for proper treatment.
Arthritis: Both osteoarthritis and rheumatoid arthritis can cause knee pain behind the knee.
Baker’s Cysts: These fluid-filled sacs form behind your knee. They can cause tightness and knee pain.
PCL Injuries: Your posterior cruciate ligament (PCL) is at the back of your knee. Injuries to this ligament cause knee pain and instability.
Tendinitis: Inflammation of tendons, like the hamstring tendons (biceps femoris tendinitis) or calf tendons (gastrocnemius tendinitis), can cause knee pain behind the knee.
Meniscus Tears: Tears in the cartilage can cause pain, especially when you bend or straighten your knee.
Leg Muscle Injuries: Hamstring strains or calf muscle injuries can cause leg pain that you feel behind your knee.
Deep Vein Thrombosis (DVT): This is a serious condition. A blood clot forms in a deep vein. It causes pain, swelling, and warmth behind the knee. Seek immediate medical treatment if you suspect DVT.
Hyperextension: Over-straightening your knee can strain the ligaments and muscles behind it. This causes knee pain.
Leg Pain Below Knee

When you feel leg pain below your knee, the specific location and characteristics of this discomfort can help you identify its cause. This area includes your shins, calves, ankles, and feet. Understanding these differences is key to finding the right solution for your leg pain.
Shin Pain
Pain in your shin, the front part of your lower leg, often comes from overuse or direct impact. You might feel a dull ache or a sharp, localized pain.
Here are common conditions that cause shin pain:
Shin splints (medial tibial stress syndrome). This is inflammation of tendons, muscles, and bone tissue around your tibia.
Minor injury to your shin, such as from a fall or blow.
Bone bruise on your shin, often from direct trauma.
Bone fracture. Your shinbone is a frequently fractured long bone.
Paget disease of the bone. In this condition, newly formed bone is abnormally shaped, weak, and brittle.
Fibrous dysplasia. Here, abnormal fibrous tissue grows in place of normal bone.
Adamantinoma and osteofibrous dysplasia (OFD). These are rare bone tumors that often affect your shinbone.
It is important to tell the difference between shin splints and a stress fracture of your tibia. Both cause leg pain, but their characteristics differ significantly.
Feature | Shin Splints | Stress Fractures |
|---|---|---|
Type of Pain | Dull, aching pain radiating along the entire length of the shin bone | Deep, throbbing pain, localized to the bone itself |
Frequency of Pain | Felt when running at top speeds | Flares up more frequently; worsens at night and while resting |
Tenderness to Touch | Pain eases away when massaging the lower leg | Pain not alleviated by massaging or putting pressure in the affected area |
Recovery | Goes away quickly; feel fine once physical activity resumes | Doesn’t go away easily; pain can still be felt while walking or running |
Another way to compare these two conditions:
Feature | Shin Splints | Stress Fracture |
|---|---|---|
Pain location | Diffuse along the inner shin | Localized to a small, pinpoint area |
Pain pattern | Dull ache during activity, improves with rest | Sharp pain that persists and worsens with activity |
Swelling | Mild and generalized | Possible and more localized |
Cause | Muscle and connective tissue overuse | Tiny crack in the bone |
Treatment | Conservative care and rest | May require immobilization or limited weight-bearing |
Diagnosis | Clinical exam, rarely imaging | Often requires X-ray or MRI |
Understanding these differences helps you seek the right treatment. Sometimes, severe shin pain can even feel like it’s radiating up towards your knee, making it seem like knee pain.
Calf Pain
Pain in your calf, the back of your lower leg, can range from a muscle cramp to a more serious condition. This type of leg pain often feels like tightness, aching, or a sharp pull.
Calf pain can also result from injuries, such as tearing of your calf muscle or tendinitis, or simply from overuse.
Here are common conditions that cause calf pain:
Varicose veins: These are swollen and twisted veins, often in your legs. Faulty valves cause them, leading to pain, throbbing, cramping, and aching.
Deep vein thrombosis (DVT): Blood clots form in your leg veins. This causes severe pain and poor leg circulation, especially after prolonged sitting or with conditions like hypertension.
Arterial claudication: A blockage in arteries supplies blood to your limbs. This causes a calf ache during exercise due to hindered blood flow.
Neurogenic claudication: A pinched nerve in your legs causes this. Lumbar spinal stenosis often causes it, affecting nerve communication and leading to calf pain (e.g., Sciatica).
Achilles tendinitis: This is inflammation of your Achilles tendon. It connects your calf muscle to your heel bone. Tension in your calf muscles often causes it, resulting in calf pain.
Compartment syndrome: This occurs after severe injury or trauma. It involves uneven distribution or build-up of blood/fluid under your skin tissue. This irritates nerves and blood vessels, causing pain, swelling, numbness, and tingling. Chronic compartment syndrome (CCS) can cause numbness, muscle bulging, or difficulty moving your foot.
Diabetic neuropathy: Nerve damage occurs due to diabetes. High blood sugar levels damage nerves (often starting in your hands and feet). This leads to numbness, tingling, and shooting pain in your calf muscles.
It is crucial to distinguish between a calf muscle strain and deep vein thrombosis (DVT). Both cause leg pain, but DVT is a medical emergency. Pain from DVT can range from a dull ache to intense throbbing, often in one leg or arm.
This discomfort frequently intensifies with prolonged walking or standing. Unlike a pulled muscle, leg pain from DVT will not go away with time. Early-stage DVT pain often starts as a dull, persistent ache that does not improve with rest or gentle stretching, typically beginning in your calf or deep in your thigh.
Consider these differences:
Duration: Calf muscle cramps are typically short-lived, fading in seconds or minutes. Pain from a blood clot persists much longer.
Swelling: Leg cramps are not usually accompanied by swelling. A blood clot in your lower leg will cause noticeable swelling.
More differentiating symptoms:
Swelling: In DVT, swelling typically occurs only in the affected leg. It usually remains even after elevation, unlike swelling from other causes.
Redness and Tenderness: These are common symptoms of DVT in the area of swelling.
Symptom Progression: DVT symptoms tend to worsen over time. Muscle strain symptoms usually resolve.
Pain Location: DVT usually causes pain in the back of your calf. An injured muscle typically causes discomfort in the side of your calf.
Symptom | Calf Muscle Strain | Deep Vein Thrombosis (DVT) |
|---|---|---|
Pain/Sensation | Tightness, intense pain (especially with stretching), tingling or burning, numbness or weakness | Pain or tenderness when standing or walking, dull ache to intense throbbing, discomfort intensifies with prolonged activity |
Swelling | Not typically mentioned as a primary symptom | Unequal swelling (one leg larger than the other), swelling usually remains even after elevation |
Skin Appearance | Not typically mentioned | Red or discolored skin, warmth |
Affected Area | General calf area | Usually affects just one leg, often in the back of the calf |
Duration/Progression | Symptoms usually resolve over time | Pain persists, symptoms tend to worsen over time, does not improve with rest or stretching |
If you suspect DVT, seek immediate medical attention. This type of leg pain requires prompt treatment. Sometimes, calf issues can alter your gait, leading to secondary knee pain.
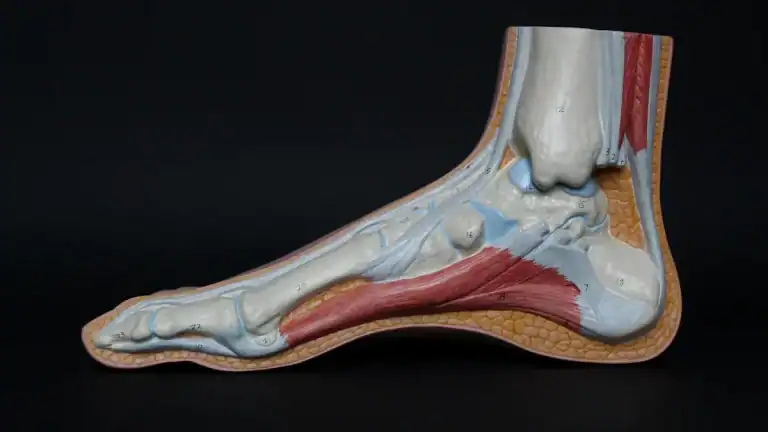
Ankle and Foot Pain
Pain in your ankle and foot can significantly impact your mobility. This leg pain can stem from various sources, from injuries to chronic conditions.
Here are common conditions that cause ankle and foot pain:
Arthritis: This is inflammation and swelling of joint cartilage and lining. Gout, an inflammatory arthritis from uric acid crystals, is one type.
Diabetes & Cardiovascular Disease related: Charcot Foot involves bone and joint damage. Diabetes-related complications, such as diabetic foot ulcer, and Peripheral Neuropathy (nerve damage) also cause issues.
Foot & Ankle Injuries: These include Bursitis (inflammation of fluid-filled sacs), Puncture Wounds, Sprains, Strains, and Fractures.
Other common causes of ankle and foot pain include:
Arthritis in your Big Toe Joint
Metatarsalgia
Morton’s Neuroma
Plantar Fasciitis and Heel Pain
Flatfoot Deformity and High Arches
Ankle Sprains
Ankle Arthritis
Achilles Tendon Ruptures
Bunions
Two common conditions causing heel and foot leg pain are Achilles Tendonitis and Plantar Fasciitis. You can differentiate them by their pain location and characteristics.
Condition | Pain Location | Pain Characteristics |
|---|---|---|
Achilles Tendonitis | Back of the heel, just above the heel bone | Pain that worsens with activity, especially running or jumping; stiffness in the Achilles tendon, particularly in the morning or after periods of rest; tenderness to the touch along the Achilles tendon; swelling or thickening of the Achilles tendon. |
Plantar Fasciitis | Bottom of the heel, often radiating into the arch of the foot | Sharp, stabbing pain in the heel, especially with the first steps in the morning or after periods of rest; pain that tends to improve with activity but may worsen again after prolonged standing or activity; tenderness to the touch on the bottom of the heel; tightness in the Achilles tendon and calf muscles. |
Understanding the specific cause of your ankle or foot leg pain helps you pursue the correct treatment. Sometimes, severe foot or ankle issues can alter your walking pattern, leading to referred knee pain.
Other Leg Pain Causes
Sometimes, your leg pain comes from issues beyond muscles or joints. These conditions can affect your whole body or specific systems. Understanding these can help you find the right treatment.
Vascular Issues
Problems with your blood vessels can cause significant leg pain. These are often called blood vessel conditions.
Peripheral Artery Disease (PAD): This is a major cause of leg pain. It affects millions of Americans. Your arteries narrow, mostly in your legs. This reduces or blocks blood flow. Plaque buildup in your arteries causes this. You might feel pain that worsens with exercise. This pain often feels like muscle cramps in your calves. It usually stops when you rest. As PAD gets worse, you can feel leg pain even when you are resting or at night.
Varicose Veins: These are swollen veins. They can also cause leg pain in your lower leg.
Leg pain is often an early sign of peripheral vascular disease (PVD). This group of conditions affects arteries, especially in your legs.
Nerve-Related Pain
Nerve pain in the leg can be sharp or burning. It happens when nerves get compressed or irritated.
Herniated Disc: The inner material of a disc in your spine can press on nearby nerves. This often leads to sciatica.
Spinal Stenosis: Your spinal canal narrows. This squeezes your spinal cord and nerves. It causes leg pain, especially when you are active.
Sciatica: This is irritation of the sciatic nerve. It causes pain that travels down your leg.
Lumbar Radiculopathy: Nerves in your lower back get compressed. This causes shooting pain, tingling, or leg numbness in your legs.
Systemic Conditions
Some conditions affect your whole body. They can lead to leg pain.
Endocrine and Metabolic Disorders: Conditions like hypothyroidism and diabetes can cause muscle and nerve damage in your legs. This leads to pain and numbness.
Charcot-Marie-Tooth disease (CMT): This genetic condition affects nerve function. It changes movement and sensation in your feet and legs.
Rheumatoid Arthritis: This autoimmune disease causes pain and inflammation in your joints.
Diabetes: This impacts your nerves and circulation. It can affect sensation and healing in your feet.
Spinal Nerve Compression
When nerves in your spine get squeezed, you can feel leg pain. This is called spinal nerve compression.
Radiculopathy: This type of spinal nerve compression causes pain that starts in your lower back. It travels down your thigh, calf, and foot. You might also feel numbness or weakness. You can also feel pins-and-needles or a warm water sensation. This usually affects only one leg.
Neurogenic Claudication: This happens when your spinal canal narrows. It causes spinal cord compression. You might feel pain and numbness in both legs when you walk or stand. Weakness during leg movements is also common. The pain often gets worse when you bend your spine backward. It improves when you bend forward, sit, or lie down.
Nerve pain is often sharp, shooting, or electric-like. It can also feel like burning. This pain can be constant or come and go.
When to Seek Medical Help
Understanding your leg pain is important. Knowing when to see a doctor is even more crucial. Some symptoms need immediate medical attention. You should never ignore these signs.
Red Flag Symptoms
Certain symptoms signal a serious problem. You need to seek immediate medical help for these.
Sudden, Severe Pain: If you experience sudden, severe leg pain, get help right away. This is especially true if you also have redness, warmth, or difficulty breathing. These could mean a blood clot or infection.
Deep Vein Thrombosis (DVT): This is a serious condition. A blood clot forms in a deep vein. Look for these signs:
Active cancer
Paralysis or recent immobilization of your leg
Recent bed rest for 3 days or major surgery within 12 weeks
Tenderness along deep veins
Your entire leg is swollen
Calf swelling is 3 cm larger than your other leg
Pitting edema (indentation when you press) in only the painful leg
Visible collateral superficial veins (not varicose)
A history of DVT
If you have leg pain with redness, warmth, and swelling, and then have trouble breathing, chest pain, or cough up blood, a clot may have moved to your lungs. This is a medical emergency.
Fractures: A recent injury, like a fall or sports injury, can cause a fracture. You might see bruising, swelling, and feel significant pain. This is especially true if you have osteoporosis.
Nerve Issues: If you suddenly lose control of your bladder or bowels, or feel weakness in both legs, you might have
cauda equina syndrome. This is a rare but serious spinal condition. It needs emergencytreatment.
Persistent or Worsening Pain
Sometimes, your leg pain is not an emergency, but it still needs attention. You should consult a doctor if your leg pain is constant. Seek help if it gets worse over time. Do not wait if it does not improve with rest and home care. This type of pain, especially if severe, needs a healthcare provider to check it. Swelling, redness, or warmth with persistent pain also means you should see a doctor.
Consulting a Doctor
You have many reasons to consult a doctor about your leg pain. They can provide a proper diagnosis. This helps you get the right treatment. Do not hesitate to seek medical advice for any persistent, severe, or concerning symptoms. Your doctor can help you understand the cause of your leg pain. They will guide you on the best path to recovery.
The Leg Pain Identifier Chart helps you with understanding leg pain. This leg pain identifier is a valuable first step for your leg discomfort. However, self-assessment has limits.