
Low blood pressure, also called hypotension, generally means your blood pressure falls below 90/60 mm Hg. However, a specific low blood pressure reading does not always signal a problem. Your optimal range is individual; it depends on your symptoms. Understanding hypotension and its potential “hypo-risks” is crucial for your health. This low blood pressure chart helps you recognize and manage hypotension effectively.
Key Takeaways
- Low blood pressure, or hypotension, means your blood pressure is below 90/60 mm Hg. Your ideal blood pressure depends on your health and symptoms.
- Watch for symptoms like dizziness, lightheadedness, or blurred vision. Seek immediate medical help for severe signs like confusion or rapid breathing.
- Many things cause low blood pressure. These include medical conditions, medications, dehydration, and sudden events like blood loss.
- Manage low blood pressure with lifestyle changes. Drink more water, eat small meals, and change positions slowly. Your doctor may prescribe medicine if needed.
- Untreated low blood pressure can cause falls, injuries, and organ damage. It can also lead to a dangerous condition called shock.
Understanding Low Blood Pressure

Defining Hypotension
You might hear the term “hypotension” when people talk about low blood pressure. This simply means your blood pressure is lower than what doctors consider normal. Generally, a blood pressure reading below 90/60 mm Hg indicates low blood pressure.
The top number, systolic pressure, measures the pressure in your arteries when your heart beats. The bottom number, diastolic pressure, measures the pressure when your heart rests between beats. While this general threshold exists, your optimal blood pressure can vary.
General Blood Pressure Thresholds
Doctors use specific numbers to define different blood pressure categories. Understanding these thresholds helps you know where your blood pressure stands.
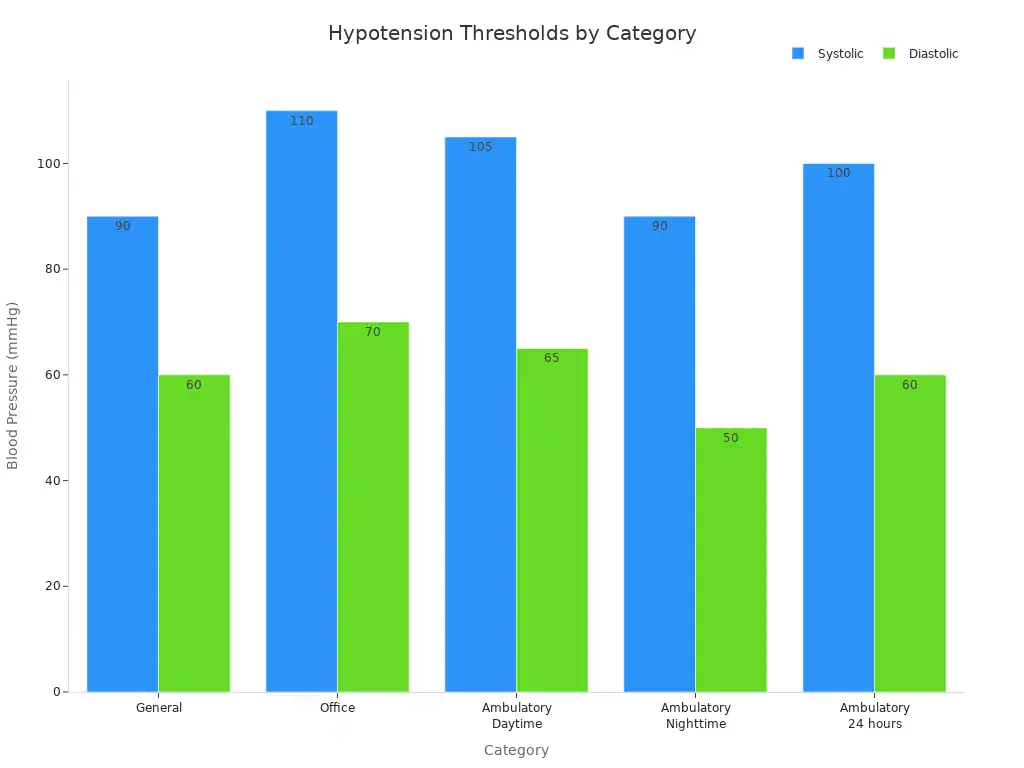
Here are some common thresholds for hypotension:
| Category | Systolic (mmHg) | Diastolic (mmHg) |
|---|---|---|
| General | <90 | <60 |
| Office | <110 | <70 |
| Ambulatory Daytime | <105 | <65 |
| Ambulatory Nighttime | <90 | <50 |
| Ambulatory 24 hours | <100 | <60 |
A Mean Arterial Pressure (MAP) below 65 mmHg also indicates hypotension. This measurement reflects the average pressure in your arteries during one cardiac cycle. In hospital settings, especially for very sick patients, doctors often use an absolute MAP threshold of 65 mmHg to define hypotension.
To give you a broader picture, here are the general categories for blood pressure, including normal and high ranges:
| Blood Pressure Category | Systolic (Top Number) | Diastolic (Bottom Number) |
|---|---|---|
| Normal | Below 120 | Below 80 |
| Elevated | 120 to 129 | Below 80 |
| Stage 1 Hypertension | 130 to 139 | 80 to 89 |
| Stage 2 Hypertension | 140 or higher | 90 or higher |
| Hypertensive Crisis | 180 or higher | 120 or higher |
Interpreting Your Readings
You need to interpret your blood pressure readings carefully. A single low blood pressure reading does not always mean you have a problem. Many factors can temporarily lower your blood pressure. These include your activity level, stress, or even the time of day.
When you monitor your blood pressure at home, follow these guidelines for accurate results:
- Avoid physical activity, caffeine, or other stimulants for 30 minutes before measurement.
- Ensure your bladder is empty.
- Rest quietly and avoid talking or texting for five minutes before and during the measurement.
- Place the cuff tautly on a bare arm, just above the antecubital fossa (the crease of your elbow).
- Position the center of the cuff over your brachial artery. Manufacturers usually mark this spot.
- Sit with your back supported, your legs uncrossed, and your feet flat on the floor.
- Rest your arm on a flat surface with the cuff at heart level.
For consistent results, take two measurements at least one minute apart, twice daily. Record these blood pressure readings for a minimum of three days, or ideally, seven days. Then, average the recorded readings. Some guidelines suggest you omit the first day’s readings because they tend to be higher.
You should use a validated, fully automated blood pressure measurement device. This device must have an appropriately sized upper arm cuff. It should also be capable of storing measurements.
You can find validated monitors on reputable websites like the U.S. Blood Pressure Validated Device Listing (https://www.validatebp.org) or The Dabl Educational Trust (http://www.dableducational.org/sphygmomanometers/devices_2_sbpm.html#ArmTable).
Comparing your home readings to office readings can also be helpful:
| Office (mm Hg) | Home (mm Hg) | 24-hour ambulatory (mm Hg) |
|---|---|---|
| 120/80 | 120/80 | 115/75 |
| 130/80 | 130/80 | 125/75 |
| 140/90 | 135/85 | 130/80 |
| 160/100 | 145/90 | 145/90 |
This low blood pressure chart helps you understand the differences. If your blood pressure readings are consistently low and you experience symptoms, you should consult a doctor.
The Optimal Blood Pressure Range

Individual Optimal Range
For most adults, a normal or optimal blood pressure is less than 120/80 mm Hg. However, your “optimal” range is truly individual. It depends on your unique health situation.
What is healthy for one person might be too low for another. You might have naturally lower blood pressure readings without any problems. This is often a sign of good cardiovascular health. The key is how you feel. If you have no symptoms of low blood pressure, your lower readings are likely fine.
Factors Influencing Your Range
Many factors influence your ideal blood pressure. Your blood pressure levels are not static. They vary based on your age and gender, along with other personal health factors.
For example, engaging in at least 150 minutes of physical activity each week helps maintain normal blood pressure. Eating a diet like the DASH (Dietary Approaches to Stop Hypertension) plan also supports healthy levels. Moderate or no alcohol intake is linked to normal blood pressure. Managing your weight, aiming for an overweight or normal weight instead of obesity, also contributes.
Other health conditions also play a role. If you have chronic conditions like heart disease or kidney disease, your optimal blood pressure target changes. For instance, if you have coronary artery disease, your diastolic pressure may need to stay above 50-55 mm Hg.
Your age is a key factor in setting personal blood pressure goals. Your overall health status helps define an acceptable blood pressure range. Even whether you experience side effects from blood pressure medication can impact your target range for hypotension.
When Low Is Not a Concern
Sometimes, low blood pressure is not a problem. If your blood pressure readings are consistently below 120/80 mm Hg but you feel fine, you likely have healthy blood pressure. Many athletes and very fit individuals have naturally low blood pressure.
This type of hypotension does not cause symptoms like dizziness or fainting. It simply means your heart and blood vessels work efficiently. You do not need to worry about low blood pressure if you have no symptoms. However, always discuss any concerns about your blood pressure with your doctor. They can help you understand your personal low blood pressure chart.
What Are the Symptoms of Low Blood Pressure?
You might wonder, what are the symptoms of low blood pressure? Many people with hypotension experience no symptoms at all. However, when symptoms do appear, they often start subtly. You need to recognize these signs.
Recognizing Mild Symptoms
When your blood pressure drops, you might first notice some mild changes. You could feel dizzy or lightheaded, especially when you stand up quickly. This feeling often passes quickly. You might also experience nausea or even vomiting. Your vision could become distorted or blurred for a moment. You may feel tired, sluggish, or generally weak. Sometimes, you find it hard to concentrate. These are common symptoms of low blood pressure.
Here are some mild symptoms you might experience:
- Dizziness or feeling lightheaded
- Nausea or vomiting
- Distorted or blurred vision
- Fatigue or weakness
- Feeling tired, sluggish, or lethargic
- Confusion or trouble concentrating
These symptoms often improve if you sit or lie down. This is especially true if you experience orthostatic hypotension.
Signs of Moderate Hypotension
When your hypotension becomes more pronounced, you experience these mild symptoms more frequently or intensely. You might notice persistent fatigue throughout the day. Your weakness could make daily tasks harder.
You might also find your skin looks pale and feels clammy. These signs indicate your body struggles to get enough blood flow. This condition is often called symptomatic hypotension. You might find relief by sitting or lying down when these feelings occur. This is especially true if you have orthostatic hypotension.
Urgent Symptoms to Watch For
You must recognize when low blood pressure becomes a medical emergency. What are the possible signs of low blood pressure that demand immediate attention?
Severe hypotension can lead to dangerous complications. Look for extreme confusion or disorientation. Your breathing might become rapid and shallow. Your pulse could feel weak and fast. Your skin may turn cold and pale. You might even lose consciousness. These are critical signs. They mean your organs are not getting enough blood and oxygen. Seek emergency medical help immediately if you experience any of these severe symptoms of low blood pressure.
Causes of Low Blood Pressure
You might ask, what causes low blood pressure? Many factors can lead to hypotension. These range from medical conditions to your daily habits. Understanding these causes helps you manage your health better.
Medical Conditions
Several medical conditions can be underlying causes of low blood pressure. Heart problems, such as a very slow heart rate or heart valve issues, reduce the amount of blood your heart pumps. This directly lowers your blood pressure. Endocrine problems, like adrenal insufficiency or thyroid conditions, also impact your blood pressure regulation.
For example, diabetes can affect your body’s ability to maintain stable blood pressure. Severe infections, known as septic shock, cause a dramatic drop in blood pressure. Allergic reactions (anaphylaxis) also lead to sudden, severe hypotension.
Medication Effects
Certain medications you take can also be causes of low blood pressure. Some drugs are designed to lower blood pressure, but they can sometimes lower it too much.
Medications known to cause low blood pressure include:
- Alpha-blockers: These can cause a drop in blood pressure, especially when you stand up.
- Diuretics: These “water pills” increase urine output, which can reduce blood volume and lead to hypotension.
- Other blood pressure medications: Taking these alongside alpha-blockers can cause a dangerous drop in blood pressure.
- Benzodiazepines or Barbiturates: These sedatives, when combined with alpha-blockers, can also lead to a dangerous drop in blood pressure.
You should always discuss your medications with your doctor. They can help you understand potential side effects.
Lifestyle and Dehydration
Your daily habits and hydration levels significantly affect your blood pressure. Dehydration is a common reason for low blood pressure. Even minor changes in your hydration can affect how your body regulates blood pressure. When you are moderately dehydrated, your blood volume decreases.
Water makes up a large part of your blood. Less blood means less oxygen and nutrients reach your tissues. Your body tries to compensate, but severe dehydration can dangerously lower your blood pressure.
This happens because it depletes essential electrolyte minerals. This destabilizes your circulatory system. This loss overwhelms your body’s protective mechanisms. It leads to hypotension, dizziness, weakness, and confusion. You might need emergency IV hydration in severe cases.
Acute Events and Hypoglycemia
Sudden events can also trigger acute hypotension. For instance, significant blood loss from an injury or internal bleeding reduces your blood volume quickly. This causes a rapid drop in blood pressure.
Severe dehydration, as mentioned, can also lead to an acute drop. Another important factor is low blood sugar, or hypoglycemia. When your blood sugar levels fall too low, your body releases hormones. These hormones can cause your blood vessels to widen, leading to a decrease in blood pressure.
Types of Low Blood Pressure
You can experience different types of low blood pressure, or hypotension. Each type happens under specific conditions. Understanding these types helps you recognize when your blood pressure drops.
Orthostatic Hypotension
Orthostatic hypotension occurs when your blood pressure drops suddenly after you stand up from sitting or lying down. Your body has mechanisms to regulate blood pressure when you change positions. For example, when you stand, gravity pulls blood into your legs and trunk. This causes a temporary decrease in blood returning to your heart. Your body usually counters this.
Muscle contractions in your legs and abdomen compress veins. One-way valves in your veins help move blood back to your heart. Your autonomic nervous system also adjusts blood vessel tone and heart rate. Baroreceptors in your carotid arteries and aorta detect drops in blood pressure.
They trigger an increase in sympathetic activity. This makes arteries constrict and your heart beat faster. Orthostatic hypotension happens when these regulatory systems fail. This can be due to low blood volume, problems with your autonomic nervous system, or your heart’s inability to pump enough blood.
Postprandial Hypotension
Postprandial hypotension is a drop in blood pressure that happens after you eat. This type of hypotension often occurs because your body sends more blood to your digestive system after a meal. Large meals are a common trigger.
Meals high in carbohydrates are also linked to this condition. Insulin release after eating high-carb foods might interfere with your autonomic nervous system. To manage this, you can try eating smaller, more frequent, low-carbohydrate meals.
Neurally Mediated Hypotension
Neurally mediated hypotension (NMH) happens when your body has an abnormal reflex. This reflex causes your blood pressure to drop. It often involves an exaggerated response from your nervous system. Abnormal stimulation of cardiac mechanoreceptors in your heart sends signals to your brainstem.
These signals then lead to increased parasympathetic activity and decreased sympathetic activity. This slows your heart rate and lowers your blood pressure. Venous pooling, where blood collects in your veins, can also trigger an exaggerated neurocardiogenic reflex. This reflex can cause your blood pressure to fall too much.
Severe Hypotension (Shock)
Severe hypotension can lead to a life-threatening condition called shock. Doctors often diagnose shock when you show signs of hypoperfusion along with low or decreasing blood pressure.
Hypoperfusion means your organs are not getting enough blood flow. While tissue hypoperfusion can happen without low blood pressure, doctors typically identify shock when you have both arterial hypotension and organ dysfunction. Key indicators include altered cognition or agitation.
Hypo-Risks and Complications
You need to understand the potential risks and complications of low blood pressure. While mild hypotension might not cause problems, severe or prolonged low blood pressure can lead to serious health issues.
Dizziness and Fainting
When your blood pressure drops too low, your brain does not get enough blood. This causes symptoms like dizziness and lightheadedness. You might feel unsteady on your feet. Sometimes, this lack of blood flow can make you faint. Fainting means you temporarily lose consciousness. This can happen suddenly and without warning.
Falls and Injuries
Dizziness and fainting directly increase your risk of falls. When you feel dizzy or faint, you can lose your balance. This leads to accidental falls. Falls can cause serious injuries, especially for older adults.
For men, low systolic blood pressure (SBP) or low diastolic blood pressure (DBP) increases the risk of falls. This is especially true for men over 70 years old. If your standing SBP is below 140 mmHg, you have a 2.8 times higher risk of falls.
Changes in your arteries can also contribute to falls. Stiff or calcified blood vessels can make it harder for your body to regulate blood pressure. This means your brain might not get enough blood when you stand or walk.
This increases your fall risk. Blood pressure dropping when you stand, known as orthostatic hypotension, strongly links to frailty and falls in older people. A faster drop in systolic blood pressure upon standing shows the strongest connection to how frail a person is and how many falls they had in the past year.
Organ Damage Risks
Your organs need a steady supply of blood to work correctly. Blood carries oxygen and nutrients. When you have prolonged or severe low blood pressure, your organs do not get enough of these vital supplies. This can damage important organs like your brain, kidneys, and heart.
Over time, this lack of blood flow can lead to permanent organ damage. You must address persistent hypotension to protect your organs.
Risk of Shock
Very severe low blood pressure can lead to a life-threatening condition called shock. Shock means your organs are not getting enough blood flow to function. This can cause your body systems to shut down.
Immediate consequences of shock include:
- Your body fluids contain too much acid (acidosis).
- You become dehydrated.
- Your kidneys or brain can suffer damage.
- Your body experiences metabolic acidosis.
- You suffer from a lack of oxygen (hypoxia).
- You could have a heart attack.
- Your circulatory system fails, leading to multiple organ failure and death.
Long-term consequences depend on your health before shock and how severe the shock was. Severe organ damage can become irreversible. You might need ongoing medical treatments.
Treatment procedures for shock can also have complications. These include circulatory overload, increased pressure in your abdomen, reactions to blood transfusions, and issues from surgical or radiological procedures.
When to Seek Medical Attention
You need to know when to seek medical attention for low blood pressure. While some low readings are normal, certain symptoms or consistent low blood pressure readings require a doctor’s visit.
Consulting Your Doctor
You should consult your doctor if you experience symptoms from known hypotension. These symptoms might affect your daily life or disrupt your routine. If you do not know you have hypotension but experience repeated dizziness or fainting, see your doctor.
These could indicate other serious health conditions. Seek medical advice if you have chest pain or if you pass out. If you fall due to lightheadedness and hit your head, especially if you take blood-thinning medications, get medical help. Also, if you injure yourself from a fall due to passing out, see a doctor.
If you show any signs of shock, such as feeling cold, sweating, rapid breathing, or a fast heart rate, consult your doctor. A bluish tint on your lips or under your fingernails also warrants a visit. Your doctor can help determine how is low blood pressure diagnosed and what your specific blood pressure readings mean.
Recognizing Emergency Signs
You must recognize critical emergency signs of dangerously low blood pressure. These signs require immediate medical help. Look for an altered mental state, such as confusion, agitation, or restlessness.
Unconsciousness also indicates a problem. These symptoms happen because your brain does not get enough blood. You might notice an abnormal heart rate or a weak pulse. Your skin could be cold, clammy, and pale. A bluish tint on your lips or extremities means oxygen deprivation.
You might also have rapid, shallow breathing. Severely low blood pressure causes dizziness and fainting. It can also lead to organ failure. Drastically reduced urine output means your kidneys struggle. Nausea, vomiting, and abdominal discomfort also signal distress. These are all signs of a severe drop in blood pressure.
Preparing for Your Visit
When you prepare for your doctor’s visit, gather important information. Write down all your symptoms. Note when they started and how often they occur. List all medications you take, including over-the-counter drugs and supplements. Bring any recent blood pressure readings you have.
If you have been doing regular blood pressure monitoring at home, bring those records. This helps your doctor understand your condition. Your doctor will ask about your medical history. They will also perform a physical exam. This information helps them understand your hypotension and create a treatment plan.
Managing Low Blood Pressure
You can manage low blood pressure, or hypotension, through various strategies. These include changes to your daily habits, dietary adjustments, and sometimes medical treatments. Understanding how is low blood pressure treated helps you take control of your health.
Lifestyle Adjustments
You can make several lifestyle changes to help manage your hypotension. Eat small, frequent meals to prevent big blood pressure drops. Increase your water intake and limit alcohol to avoid dehydration.
When you exercise outdoors in hot weather, take frequent breaks and hydrate more. Avoid long exposure to saunas, hot tubs, and steam rooms. These can dehydrate you. Change your body positions slowly, especially when you stand up. Avoid long periods of bed rest. You can also wear compression stockings. These help blood circulate from your legs and feet.
Dietary Considerations
Your diet plays a big role in managing low blood pressure. Drink plenty of fluids, at least two liters or eight glasses of water daily. Drink more in hot weather or during exercise. This prevents reduced blood volume from dehydration. You can eat salty foods like olives, cottage cheese, or canned soup. You can also add salt to your meals. High salt content can raise blood pressure.
Drink caffeine, like coffee or tea, to temporarily increase your heart rate and blood pressure. Boost your B12 intake with foods like eggs, chicken, and salmon. This helps produce healthy red blood cells.
Fill up on folate from asparagus, broccoli, and lentils. Cut back on carbohydrates, especially processed ones. Their quick digestion can cause sudden blood pressure drops. Eat smaller, more frequent meals instead of large ones. This prevents blood pressure from plunging during digestion.
You now understand what constitutes low blood pressure. Your optimal range is individual. You also know the potential hypo-risks of hypotension.
Recognizing symptoms is important. Understand when to seek professional medical advice for your hypotension. While low blood pressure can be benign, you must monitor and manage your hypotension, especially if symptoms are present. This low blood pressure chart helps you.


