
Red blood cells, also known as erythrocytes, are crucial for delivering oxygen to the body’s tissues through the circulatory system. They absorb oxygen in the lungs and release it into tissues as they navigate through capillaries. A low red blood cell count means the body does not have enough of these vital cells. This condition is explicitly called anemia.
Nearly 1 in 4 people worldwide, or approximately 2 billion individuals, are affected by anemia annually. A low RBC count is a symptom of an underlying issue, not a disease itself. It increases the risk of developing anemia, which often requires various Treatment Options.
Key Takeaways
Red blood cells carry oxygen to your body. A low count means your body does not get enough oxygen.
Many things can cause a low red blood cell count. These include not eating enough healthy foods, losing blood, or having long-term sicknesses.
Symptoms of a low red blood cell count include feeling tired, dizzy, or short of breath. Your skin might also look pale.
A low red blood cell count can be dangerous. It can harm your organs and heart if not treated.
You can treat a low red blood cell count. Eating healthy foods, taking medicine, or getting blood transfusions can help.
What Are Red Blood Cells
Red blood cells, or erythrocytes, are tiny, disc-shaped cells in the blood. Their primary job involves carrying oxygen from the lungs to every part of the body. They also transport carbon dioxide back to the lungs for exhalation. Hemoglobin, a protein rich in iron, gives red blood cells their color and allows them to bind with oxygen. Without enough red blood cells, the body’s tissues and organs do not receive the oxygen they need to function correctly. This lack of oxygen delivery leads to the symptoms and dangers associated with a low RBC count.
Normal RBC Ranges
Healthcare providers use specific ranges to determine if a person’s red blood cell count is healthy. These ranges can vary based on age and sex. A count below these normal levels indicates a low RBC count.
Category | Red Blood Cell Count (10*6/uL) |
|---|---|
Adult Males | 4.60 – 6.10 |
Adult Females | 4.00 – 5.40 |
Children (0-13 days) | 4.00 – 6.60 |
Children (14-30 days) | 3.60 – 6.20 |
Children (1-2 months) | 3.00 – 5.40 |
Children (3-5 months) | 3.10 – 4.50 |
Children (6 months – 1 year) | 3.70 – 5.30 |
Children (2-5 years) | 3.90 – 5.30 |
Children (6-11 years) | 4.00 – 5.20 |
Children (12-17 years, Male) | 4.50 – 5.30 |
Children (12-17 years, Female) | 4.10 – 5.10 |

Diagnosing Low RBC Count
Doctors diagnose a low red blood cell count through various laboratory tests. These tests help identify the presence of anemia and its underlying cause.
Complete Blood Count (CBC): This initial test measures red blood cells, white blood cells, hemoglobin, and platelets. Doctors specifically look at red blood cell and hemoglobin levels. Mean corpuscular volume (MCV) from a CBC can also suggest types of anemia.
Iron Panel: If iron deficiency is a possibility, this test measures iron levels in the blood. It includes values like ferritin, serum iron, and transferrin saturation.
Reticulocyte Count: This test measures immature red blood cells. It shows if the bone marrow produces enough new red blood cells.
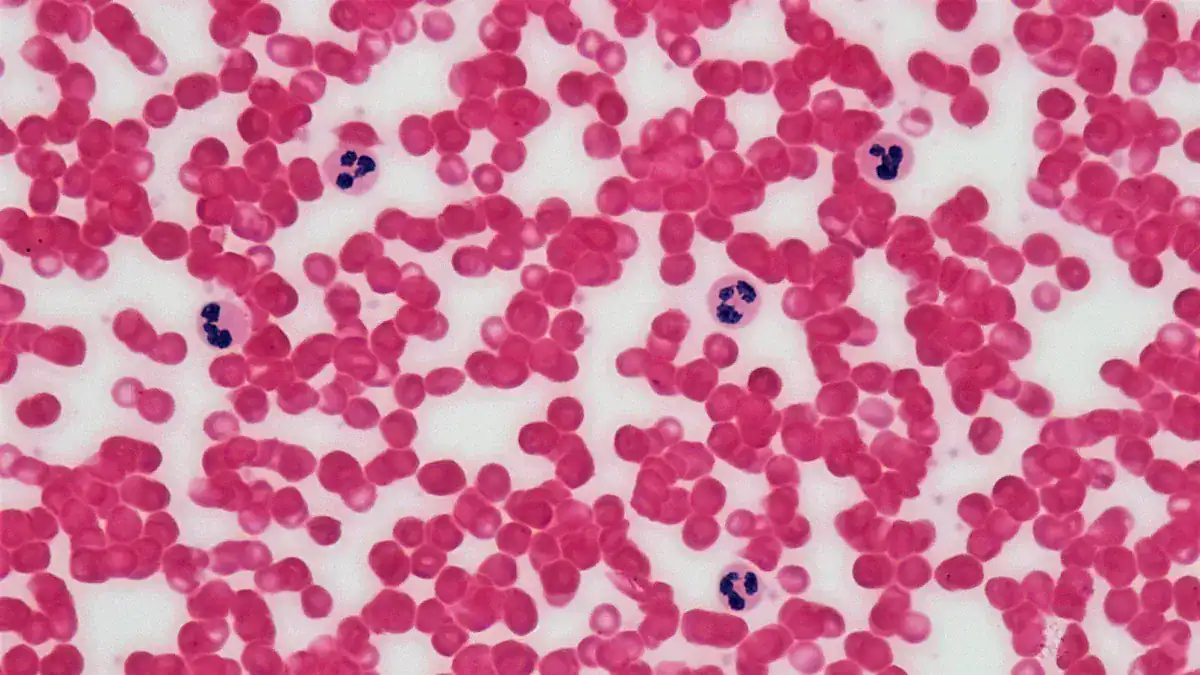
Blood Smear: A technician examines a blood sample under a microscope. This helps identify abnormal cell shapes, which can point to specific conditions like sickle cell anemia.
Other Tests: Doctors may order additional tests for specific types of anemia. These include:
Lactate Dehydrogenase (LDH) test and Haptoglobin test for hemolytic anemia.
Vitamin B12 and Folate Levels to check for vitamin deficiencies.
Coombs Test if an autoimmune disease is suspected.
Causes of Low RBC Count
Many factors can lead to a low red blood cell count. These causes range from dietary issues to serious medical conditions. Understanding these causes helps in finding the right Treatment Options.
Nutritional Deficiencies
The body needs specific nutrients to produce healthy red blood cells. A lack of these nutrients can significantly reduce RBC count.
Iron-deficiency anemia is the most common type. Iron is essential for making hemoglobin, the protein in red blood cells that carries oxygen.
Low levels of folate (vitamin B9) can also cause this condition. Folate helps in the production of new red blood cells.
Similarly, low levels of vitamin B-12 hinder proper red blood cell formation.
A low vitamin C intake can contribute to iron deficiency because vitamin C helps the body absorb iron.
Blood Loss
Losing blood, whether suddenly or over time, directly reduces the number of red blood cells.
Acute blood loss can happen from injuries, surgery, or childbirth.
Chronic blood loss often occurs internally. This can be due to conditions like stomach ulcers, hemorrhoids, or heavy menstrual bleeding. Gastrointestinal bleeding, even if minor, can lead to significant RBC loss over time.
Chronic Illnesses
Several long-term health conditions can suppress red blood cell production or increase their destruction.
Cancer is a frequent cause. Blood cancers like leukemia and lymphoma directly affect bone marrow function. Other cancers, such as cervical cancer and colon cancer, can cause chronic blood loss. Cancer treatments like chemotherapy and radiation also damage bone marrow.
Chronic Kidney Disease often leads to low RBC counts. Kidneys produce erythropoietin, a hormone that stimulates red blood cell production. Damaged kidneys produce less of this hormone.
Autoimmune diseases cause inflammation throughout the body. Conditions like Crohn’s disease, systemic lupus erythematosus, rheumatoid arthritis, and ulcerative colitis can lead to anemia of chronic disease.
Long-term infections also contribute to low RBC counts. Examples include bacterial endocarditis, osteomyelitis, HIV/AIDS, lung abscess, hepatitis B, and hepatitis C.
Heart failure (congestive heart failure) and obesity are also linked to lower RBC counts.
Bone Marrow Issues
The bone marrow is the body’s factory for blood cells. Problems with bone marrow can severely impact red blood cell production.
Aplastic anemia occurs when the bone marrow cannot produce enough blood cells. Damage to stem cells within the bone marrow reduces the number of various blood cell types, including red blood cells.
Myelodysplastic syndromes are a group of disorders where the bone marrow produces abnormal blood cells that do not mature properly. This leads to an insufficient production of healthy blood cells.
Some inherited conditions directly affect bone marrow function. Diamond-Blackfan anemia is an example where the bone marrow fails to produce enough stem cells.
Fanconi anemia is another inherited condition. It causes bone marrow failure, impairing the production of all blood cells, including red blood cells. This leads to extreme tiredness due to anemia.
Red Blood Cell Destruction
Sometimes, the body destroys red blood cells faster than it can produce them. This process is called hemolysis.
Extravascular hemolysis happens when macrophages, mainly in the spleen, liver, and bone marrow, remove red blood cells prematurely. This occurs because the red blood cells are abnormal or have antibodies attached.
Intravascular hemolysis means red blood cells “pop” directly in the bloodstream. This releases hemoglobin into the plasma and urine.
Defective red blood cells can be a cause. Structural irregularities, often inherited, make red blood cells fragile. Examples include unstable hemoglobins (like in sickle cell anemia and thalassemia), enzyme deficiencies (e.g., G6PD deficiency), and membrane defects (e.g., hereditary spherocytosis).
Immune system-related conditions can cause the immune system to attack red blood cells. This happens in autoimmune hemolytic anemia. Underlying conditions like Mycoplasma pneumonia, lymphoma, leukemia, lupus, and rheumatoid arthritis can trigger this.
Infections can also damage red blood cells. Malaria, Babesiosis, and HIV are examples.
Certain medications can induce immune hemolytic anemia. Acetaminophen, cephalosporins, penicillin, and sulfonamides are some examples.
Pregnancy complications like HELLP syndrome, preeclampsia, and eclampsia can lead to premature red blood cell breakdown.
Rarely, medical devices and treatments such as hemodialysis can cause hemolysis.
Inherited Conditions
Genetic factors play a role in several conditions that cause low RBC counts.
Iron-refractory iron-deficiency anemia is a genetic form of iron deficiency. Iron supplements do not effectively increase iron levels in these cases.
Sickle cell anemia is a common inherited blood disorder. It affects hemoglobin, causing red blood cells to become crescent-shaped. These cells break down rapidly.
Thalassemia is a group of conditions similar to sickle cell disease. They impact the hemoglobin protein, leading to reduced RBC production and increased destruction.
Pregnancy and Other Factors
Pregnancy naturally increases blood volume, which can dilute the red blood cell count. This often leads to physiological anemia. Other factors like chronic alcohol abuse, exposure to certain toxins, and some medications can also contribute to a low RBC count.
Symptoms of Low RBC Count
A low red blood cell count often causes noticeable symptoms. These signs appear because the body does not receive enough oxygen. Recognizing these symptoms helps individuals seek timely medical attention.
Fatigue and Weakness
Fatigue is one of the most common symptoms of anemia. Individuals often feel very tired and weak. This exhaustion can persist even after adequate rest. The body struggles to transport sufficient oxygen without healthy red blood cells. This makes everyday tasks challenging. Other common symptoms include:
Fatigue
Dizziness
Shortness of breath
Heart palpitations
Shortness of Breath
People with a low RBC count may experience shortness of breath. This happens because the blood cannot carry enough oxygen to the lungs and other tissues. Even mild physical activity can trigger this symptom.
Dizziness and Lightheadedness
Reduced oxygen supply to the brain causes dizziness and lightheadedness. Individuals might feel faint, especially when standing up quickly. This symptom indicates the brain is not getting the oxygen it needs.
Pale Skin
The hemoglobin in red blood cells gives skin its healthy, rosy color. When red blood cell counts are low, the skin often appears pale. This paleness is particularly noticeable in the face, inside the eyelids, and on the nails.
Cold Extremities
Poor circulation and reduced oxygen delivery can make hands and feet feel cold. The body prioritizes oxygen for vital organs, leaving less for the extremities. This often results in a constant cold sensation.
Headaches and Chest Pain
Some individuals with a low RBC count experience headaches. This occurs due to insufficient oxygen reaching the brain. In severe cases, chest pain can develop. The heart works harder to pump oxygen-poor blood, straining the cardiovascular system. This can lead to discomfort or pain in the chest.
Dangers of Low RBC Count
A low red blood cell count can lead to serious health problems. It affects many parts of the body. Recognizing these dangers helps people understand the importance of proper care.
Organ Impairment
Red blood cells deliver oxygen to the body’s tissues and vital organs. They carry oxygen from the lungs. The amount of oxygen organs receive depends on the number of red blood cells and their quality. Anemia means not enough properly working red blood cells exist. This causes a lack of oxygen in the body. This oxygen shortage can cause weakness, shortness of breath, dizziness, and a fast heartbeat. These signs show that vital organs do not get enough oxygen.
Heart Complications
A low red blood cell count makes the heart work harder. The heart must pump more blood to deliver enough oxygen. This extra effort can strain the heart over time. It can lead to an enlarged heart or even heart failure.
Pregnancy Risks
A low red blood cell count during pregnancy poses risks for both mother and baby. For the mother, severe cases can lead to heart failure. There is also a greater risk of blood loss during labor. Mothers may also have difficulty fighting infections. For the baby, there is an increased risk of anemia in infancy. Babies face a greater risk for preterm delivery and low birth weight. The baby’s organs may not get enough oxygen. This can cause heart failure or abnormal fluid buildup in multiple body areas for the fetus.
Developmental Concerns
Anemia, especially from iron deficiency, can cause lasting developmental problems in children. Children with iron-deficiency anemia often show cognitive or developmental issues. Even mild anemia affects a child’s energy levels. It also impacts their ability to focus and learn. Chronic iron deficiency anemia can lead to permanent developmental impairment.
Increased Infection Risk
A low red blood cell count can weaken the immune system. The body becomes less able to fight off infections. This makes individuals more prone to illness.
Reduced Quality of Life
The symptoms of a low RBC count significantly reduce a person’s quality of life. Constant fatigue, weakness, and shortness of breath make daily activities difficult. This impacts work, social life, and overall well-being. Addressing the underlying cause through appropriate Treatment Options can improve life quality.
Low RBC Count Treatment Options

Addressing a low red blood cell count involves various strategies. These include medical interventions, dietary changes, and lifestyle adjustments. The specific Treatment Options depend on the underlying cause and how severe the condition is. Mild cases might not require extensive treatment.
Dietary Adjustments
Eating the right foods helps the body produce more red blood cells. Focusing on nutrients essential for blood production is key.
Nutrient | RDA (Males 19-50 years) | RDA (Females 19-50 years) | Role in RBC Production |
|---|---|---|---|
Iron | 8 mg/day | 18 mg/day | Essential for RBC production; deficiency causes anemia |
Vitamin C | 90 mg/day | 75 mg/day | Enhances iron absorption |
Copper | 900 mcg/day | 900 mcg/day | Linked to RBC production; aids iron access |
Vitamin A | 900 mcg/day | 700 mcg/day | Helps iron get to RBCs |
Vitamin B12 | 2.4 mcg/day (14+ years) | 2.4 mcg/day (14+ years) | Crucial for RBC formation |
Vitamin B9 (Folate) | 400 mcg DFE/day (14+ years) | 400 mcg DFE/day (14+ years) | Supports cell division and growth, including RBCs |
Vitamin B6 | 1.3 mg/day | 1.3 mg/day | Important for synthesizing hemoglobin |
Vitamin E | 15 mg/day (14+ years) | 15 mg/day (14+ years) | May help protect blood cells from damage |
To increase red blood cell count, dietary adjustments should include foods rich in:
Iron: This nutrient is crucial for hemoglobin. You can find it in spinach, lentils, and red meat.
Folic Acid (Vitamin B9): This supports rapid cell division and growth, including red blood cell formation. Dairy products, eggs, and fortified cereals contain folic acid. Other sources include enriched breads, dark leafy greens like kale and spinach, liver, Brussels sprouts, and asparagus.
Vitamin B12: This works with folic acid for accurate cell replication in red blood cells. Dairy products, eggs, and fortified cereals provide vitamin B12. Meat, poultry, fish, and fortified nutritional yeasts also contain it.
Copper: This aids in iron absorption, which is necessary for hemoglobin. Foods high in copper include shellfish, liver and other organ meats, whole grain products, wheat bran cereals, chocolate, nuts, and seeds.
Vitamin A: This supports the development of stem cells into mature blood cells. Carrots, sweet potatoes, spinach, dairy products, fish, eggs, liver, and tomato products are good sources.
Hydration: Staying hydrated is essential for producing healthy blood cells. Dehydration can lower blood volume and reduce RBC count.
If you have anemia, consider limiting your intake of:
Dairy products
Alcohol
Tea and coffee
Pomegranate juice
Dark chocolate
Red wine grapes
Additionally, spacing out meals can help prevent issues with nutrient absorption.
Nutritional Supplements
When diet alone is not enough, doctors may recommend nutritional supplements. These supplements provide concentrated doses of the nutrients needed for red blood cell production.
Vitamin B9 (folic acid): This is essential for red blood cell production.
Iron: This is a crucial component of hemoglobin.
Vitamin B12: This aids in the formation of red blood cells.
Copper: This helps in hemoglobin synthesis.
Vitamin A: This contributes to red blood cell formation.
Vitamin C: This facilitates iron metabolism, which is vital for hemoglobin production.
Vitamin E: This protects red blood cells from damage.
Medications
Doctors prescribe various medications to treat a low red blood cell count, depending on the cause.
Iron supplements, such as ferrous sulfate, ferric sulfate, ferrous gluconate, and ferric citrate, help increase iron levels.
Intravenous (IV) iron therapy delivers iron directly into the bloodstream for faster absorption.
Erythropoiesis-stimulating agents (ESA) encourage the bone marrow to produce more red blood cells.
Vitamin B12 injections or oral supplements treat B12 deficiency.
Corticosteroids and other immunosuppressant drugs address underlying autoimmune conditions that destroy red blood cells.
Chemotherapy drugs treat cancers that affect blood cell production.
Antibiotics treat infections that contribute to anemia.
Jesduvroq tablets represent a new oral treatment for anemia caused by chronic kidney disease.
Blood Transfusions
Blood transfusions provide a quick way to increase red blood cell count in severe cases. They are a short-term therapy. Doctors recommend blood transfusions when a patient has anemia due to a low red blood cell count, leading to symptoms such as tiredness and shortness of breath.
For hospitalized adult patients who are hemodynamically stable, a restrictive red blood cell transfusion strategy is recommended when the hemoglobin concentration is less than 7 g/dL. This also applies to hospitalized adult patients with hematologic and oncologic disorders. For critically ill children and hospitalized children at risk of critical illness who are hemodynamically stable, a restrictive transfusion strategy is recommended when the hemoglobin level is less than 7 g/dL. This excludes children with transfusion-dependent hemoglobinopathy, cyanotic cardiac conditions, or severe hypoxemia. For hemodynamically stable children with congenital heart disease, the transfusion threshold depends on the cardiac abnormality and stage of surgical repair. It is 7 g/dL for biventricular repair, 9 g/dL for single-ventricle palliation, or 7 to 9 g/dL for uncorrected congenital heart disease. Transfusion decisions should consider symptoms as well as hemoglobin concentrations.
Addressing Underlying Conditions
Treating the root cause of a low red blood cell count is often the most effective long-term solution. Many conditions can lead to anemia.
Iron deficiency anemia results from insufficient iron for hemoglobin production. This often happens due to poor diet or blood loss.
Vitamin B12 deficiency anemia occurs from inadequate B12 intake or absorption issues.
Megaloblastic anemia is triggered by B12 or B9 (folate) vitamin deficiency. This leads to unusually large red blood cells.
Pernicious anemia is a type of anemia that reduces the absorption of dietary vitamin B12.
Anemia of inflammation, also known as anemia of chronic disease (ACD), affects individuals with conditions that cause inflammation. These include infections, autoimmune diseases, cancer, and chronic kidney disease (CKD).
Other common underlying conditions include acute or chronic blood loss, bone marrow problems, certain medications like chemotherapy drugs, excessive alcohol consumption, and immune system-related destruction of red blood cells.
Effective Treatment Options for these underlying issues can resolve the low red blood cell count.
Preventing Low RBC Count
Preventing a low red blood cell count involves proactive steps. These steps focus on diet, regular health monitoring, managing existing conditions, and healthy lifestyle choices.
Balanced Diet
A balanced diet provides essential nutrients for red blood cell production. People should include foods rich in iron, vitamin B12, and folate.
Iron-rich foods:
Heme iron sources: Beef, chicken, clams, eggs, lamb, ham, turkey, veal, pork, liver, shrimp, tuna, sardines, haddock, mackerel, oysters, and scallops.
Non-heme iron sources: Dried or canned peas and beans, lentils, tofu, enriched breads and cereals, figs, dates, raisins, prunes, broccoli, dark leafy greens, potatoes, and nuts.
Folate and Vitamin B12-rich foods: Brussels sprouts, broccoli, nuts and seeds (walnuts, flax seeds), beef liver, wheat germ, papaya, bananas, and avocado.
Regular Check-ups
Regular check-ups help monitor red blood cell counts. A Complete Blood Count (CBC) is often part of routine physical exams. This test checks red blood cell levels. The frequency of blood tests varies. It depends on a person’s overall health and family medical history. Individuals with known blood disorders or chronic conditions like kidney disease may need more frequent monitoring. Doctors adjust the testing schedule based on the specific condition and treatment plan.
Managing Health Conditions
Effectively managing existing health conditions prevents a low red blood cell count. Chronic illnesses, such as kidney disease or autoimmune disorders, can affect red blood cell production. Following treatment plans for these conditions helps maintain healthy blood cell levels. This proactive management reduces the risk of developing anemia.
Lifestyle Choices
Certain lifestyle choices positively impact red blood cell count and overall health.
Exercise: Regular physical activity stimulates the body’s natural production of red blood cells. This improves oxygen transport.
Hydration: Drinking plenty of water helps maintain normal blood viscosity.
Moderating Alcohol Consumption: Excessive alcohol intake impairs red blood cell production. It can also lead to deficiencies in vital nutrients. Limiting alcohol helps prevent anemia.
Nutrient-Rich Diet: A well-balanced diet rich in iron, folic acid, and vitamin B12 supports robust red blood cell levels. This ensures optimal oxygen delivery and overall vitality.
Red blood cells play a critical role in oxygen transport, vital for overall health. A low count can lead to anemia, stemming from various causes like nutritional deficiencies, blood loss, or chronic illnesses. This condition poses dangers, including organ impairment and heart complications. Fortunately, many treatment options exist, from dietary adjustments and supplements to medications and transfusions. Early detection, accurate diagnosis, and proper management are crucial. They prevent severe complications and improve health outcomes. Always consult a healthcare professional for any suspected symptoms or concerns about a low RBC count. They provide personalized advice and care.
FAQ
What does a low RBC count indicate?
A low red blood cell count indicates the body does not have enough oxygen-carrying cells. This condition is called anemia. It often signals an underlying health issue. Doctors investigate the cause to provide proper treatment.
What are the main symptoms of a low RBC count?
Individuals with a low red blood cell count often experience fatigue and weakness. They may also feel dizzy or short of breath. Pale skin and cold hands or feet are common signs. Headaches and chest pain can also occur.
What foods help increase red blood cells?
Eating foods rich in iron, vitamin B12, and folate helps increase red blood cells. Examples include red meat, spinach, lentils, and fortified cereals. Vitamin C-rich foods, like oranges, also aid iron absorption.
What are the dangers of an untreated low RBC count?
An untreated low red blood cell count can lead to serious health problems. It can impair organ function and strain the heart. This may result in heart complications. It also increases infection risk and reduces overall quality of life.




