Dermatomes are specific skin areas. A single spinal nerve innervates each dermatome. These sensory maps are critical for neurological assessment and diagnosis. Understanding these dermatomes helps identify nerve problems. Conditions affecting these nerve pathways are common.
Lumbar radiculopathy affects 3-5% of the population. About 12-40% of people with back pain experience radiculopathy symptoms. Symptomatic lumbar disc herniations affect 1-3% of the general population.
This blog focuses on lumbar dermatomes L1-L5. They map sensation in the lower body. This guide provides a clear dermatome map for diagnostic and educational purposes.
Key Takeaways
Dermatomes are specific skin areas. A single spinal nerve connects to each area. These nerves send feelings like touch and pain to your brain.
Doctors use dermatome maps. These maps help them find nerve problems. They look at where you feel pain or numbness.
Lumbar dermatomes L1-L5 cover your lower back, buttocks, thighs, and shins. Each one links to a specific nerve in your spine.
If a lumbar dermatome is hurt, you might feel pain, numbness, or tingling. These feelings happen in the skin area linked to that nerve.
Understanding Lumbar Dermatomes
Dermatome Definition and Function
A dermatome is a specific area of skin. Afferent nerve fibers primarily supply this skin area. These fibers come from the dorsal root of a single spinal nerve. These nerves relay sensations, including pain, from that skin region to the brain. Dermatomes function like a map.
They show areas of skin on the body. These areas rely on specific nerve connections on the spine. Each dermatome corresponds to a specific segment of the spinal cord. Sensory information from these areas travels through sensory nerve fibers. These fibers go to their respective spinal segments.
A single spinal nerve provides sensation to specific skin areas, including dermatomes. Spinal nerves are part of the peripheral nervous system (PNS). The PNS connects the body to the central nervous system (CNS). Each dermatome links to a single spinal nerve. This nerve transmits sensations, such as pain, from that specific skin area to the CNS.
Clinical Importance of Dermatomes
Dermatome maps are crucial diagnostic tools. Doctors use them to assess potential spinal nerve involvement. They look at the location of pain, numbness, or tingling. Further testing is often needed to confirm a diagnosis. Dermatome maps help track conditions like shingles. The rash and pain of shingles follow a dermatome pattern. This helps in diagnosis.
Doctors also use sensory tests to evaluate nerve function in different dermatomes. These tests include pinprick, light touch, and temperature tests. Knowledge of dermatomes guides targeted treatments. Doctors confirm diagnoses and plan treatments.
These treatments include nerve blocks or steroid injections. They target the exact area causing pain. Anesthesiologists use dermatome maps to plan regional anesthesia. This includes epidural and spinal anesthesia for surgeries. Dermatome knowledge is vital for nerve blocks. Doctors inject numbing medicine near specific nerves. This blocks pain signals along particular dermatomes.
Spinal Nerves and Sensory Pathways
The human body has 31 pairs of spinal nerves. These nerves supply dermatomes. Individual sensory neurons from dermatomes bundle into spinal nerves. These spinal nerves enter the spinal cord through its posterior root or horn. Each spinal nerve carries information from a specific skin region called a dermatome.
A dermatome is an area of skin. Peripheral nerve fibers supply this area. These fibers come from a single dorsal root ganglion. Sensory information from the body goes to the CNS through the dorsal roots.
Axons from dorsal root ganglion cells are primary sensory afferents. They act as the first-order sensory neurons. The dorsal horn of the spinal cord receives and processes incoming somatosensory information. Ascending projections then emerge from the dorsal horn.
They transmit this sensory information to the midbrain and diencephalon. Spinal nerves are part of the PNS. They transmit sensory information from the periphery to the CNS. Somatic afferent fibers carry sensory information. This information comes from the skin, joints, and muscles.
These fibers pass through the dorsal root ganglion. They then transmit this information to the posterior/dorsal column of gray matter in the spinal cord. Dermatomes are defined skin areas. The sensory component of a spinal nerve distributes to a specific spinal cord segment. This relays sensory information back to the CNS through spinal nerves.
Lumbar Spine and Dermatome Overview

Regions of the Spinal Column
The spinal column is a complex structure. It protects the spinal cord and supports the body. It consists of distinct anatomical regions. From top to bottom, these regions include:
Cervical spine (neck): This section has 7 vertebrae (C1–C7).
Thoracic spine (chest/upper back): This part contains 12 vertebrae (T1–T12).
Lumbar spine (lower back): This region includes 5 vertebrae (L1–L5).
Sacrum (pelvis region): This forms from 5 fused vertebrae (S1–S5).
Coccyx (tailbone): This consists of 3–5 fused vertebrae. The lumbar spine is the focus here. It sits in the lower back. It supports much of the body’s weight. The lumbar segments are crucial for lower body sensation and movement.
General Lumbar Dermatome Distribution
The lumbar dermatomes cover specific areas of the lower body. These areas include the lower back, buttocks, thighs, and shins. Each lumbar dermatome corresponds to a specific spinal nerve. These spinal nerves transmit sensory information from the skin. For example, the L1 spinal nerve provides sensation to the groin and genital regions. The L2, L3, and L4 spinal nerves provide sensation to the front part of the thigh and the inner side of the lower leg.
The L5 spinal nerve provides sensation to the outer side of the lower leg, the upper part of the foot, and the web-space between the first and second toe. Understanding this dermatome map helps clinicians identify nerve issues. Each dermatome acts as a sensory landmark.
Doctors use these dermatomes to pinpoint nerve root compression or damage. This knowledge is vital for diagnosing conditions affecting the lower body.
L1 Lumbar Dermatome: Hip and Groin
L1 Nerve Root
The L1 nerve root originates from the spinal cord at the L1 spinal segment. It forms from the union of two distinct roots. The posterior, or dorsal, root contains sensory fibers. These fibers transmit sensations from the skin to the spinal cord. The anterior, or ventral, root consists of motor fibers. These fibers carry signals for muscle movement. These two roots merge.
They form the L1 spinal nerve at the intervertebral foramen. This nerve is one of the crucial spinal nerves that contribute to the lumbar plexus. It plays a vital role in providing sensation to specific areas of the lower body.
L1 Sensory Distribution
The L1 dermatome covers specific skin areas. Posteriorly, this dermatome includes the skin lateral to the L1 vertebra. Anteriorly, the L1 dermatome wraps around to the groin and pelvic girdle area.
It specifically overlies the inguinal canal. The inguinal region, commonly known as the groin, serves as a key dermatome landmark for L1. This area includes the upper inner thigh and parts of the genital region. Understanding this specific sensory distribution helps clinicians. They can pinpoint the exact location of a nerve issue. This dermatome provides sensory input from these regions.
L1 Clinical Presentations
L1 nerve involvement can lead to various symptoms. Patients often experience pain and paresthesia in the proximal anterolateral thigh. Paresthesia describes abnormal sensations like tingling or prickling.
Pain and paresthesia also commonly occur in the groin area. Some individuals report pain and numbness in the buttock. Another common presentation is meralgia paresthetica-like pain. This condition involves burning pain and numbness in the outer thigh.
It happens when the lateral femoral cutaneous nerve becomes compressed. While meralgia paresthetica is a distinct condition, L1 radiculopathy can mimic its symptoms due to the overlapping sensory distribution. Assessing the L1 dermatome helps doctors diagnose conditions affecting this nerve.
L2 Lumbar Dermatome: Upper Thigh
L2 Nerve Root
The L2 nerve root emerges from the spinal cord at the L2 spinal segment. It forms from the combination of sensory and motor fibers. The sensory fibers carry information from the skin.
The motor fibers send signals for muscle movement. These fibers join together. They create the L2 spinal nerve. This nerve exits the spinal column through the intervertebral foramen between the L2 and L3 vertebrae. The L2 nerve contributes to the lumbar plexus. This network of nerves serves the lower limbs and abdominal wall. This specific nerve plays a vital role in sensation and movement for the upper thigh.
L2 Sensory Distribution
The L2 dermatome covers a distinct area of the upper thigh. This dermatome provides sensation to the skin over the upper anterior thigh. It also includes the middle and lateral aspects of the anterior thigh.
This area extends from the hip region down towards the knee. Understanding this specific sensory map helps clinicians. They can identify the precise location of a nerve issue. This dermatome acts as a key indicator for problems affecting the L2 spinal nerve. The L2 dermatome is one of several dermatomes that map sensation in the lower body.
L2 Clinical Presentations
Involvement of the L2 nerve can cause various symptoms. Patients often experience pain in the anterior medial thigh. They may also report sensory changes. These changes include numbness or tingling in the upper thigh. A doctor assesses these symptoms. This helps them pinpoint the affected nerve.
Deficit Type | Presentation |
|---|---|
Pain | Anterior medial thigh |
Sensory Deficit | Upper thigh |
Motor Deficit | Slight quadriceps weakness; hip flexion; thigh adduction |
Reflex Deficit | Slightly diminished suprapatellar |
Patients can also show motor deficiencies. These affect the iliopsoas, quadriceps femoris, and hip adductor muscles. They might have difficulty lifting their leg or straightening their knee. Sensory alteration often radiates into the anterior and anterolateral thigh.
This indicates a problem with the L2 nerve. These clinical signs help doctors diagnose conditions like radiculopathy. Radiculopathy occurs when a nerve root becomes compressed or irritated. Assessing the L2 dermatome helps confirm the diagnosis. This allows for targeted treatment.
L3 Lumbar Dermatome: Mid-Thigh and Knee
L3 Nerve Root
The L3 nerve root originates from the spinal cord at the L3 spinal segment. It forms from both sensory and motor fibers. Sensory fibers carry information from the skin. Motor fibers transmit signals for muscle movement. These fibers combine to create the L3 spinal nerve. This nerve exits the spinal column through the intervertebral foramen between the L3 and L4 vertebrae. The L3 nerve contributes to the lumbar plexus. This network of nerves serves the lower limbs. It plays a significant role in sensation and movement for the mid-thigh and knee.
L3 Sensory Distribution
The L3 dermatome covers a distinct area of the lower limb. This dermatome provides sensation to the skin over the mid-thigh. It also includes the medial aspect of the knee. The L3 dermatome extends down the medial side of the thigh. It reaches the medial condyle of the femur. Understanding this specific sensory map helps clinicians. They can identify the precise location of a nerve issue. This dermatome acts as a key indicator for problems affecting the L3 spinal nerve. This specific dermatome is one of several dermatomes that map sensation in the lower body.
L3 Clinical Presentations
L3 radiculopathy is characterized by various lower limb pain and neurological deficits. Involvement of the L3 nerve can cause several symptoms. Patients often experience pain in the mid-thigh. They may also report sensory changes. These changes include numbness or tingling in the medial knee and mid-thigh. A doctor assesses these symptoms. This helps them pinpoint the affected nerve.
Here is a breakdown of common neurological symptoms associated with L3 nerve root pathology:
Symptom | Number of Patients |
|---|---|
Thigh pain | 12 |
Hip or knee pain | 5 |
Sensory disturbance | 9 |
Motor weakness | 2 |
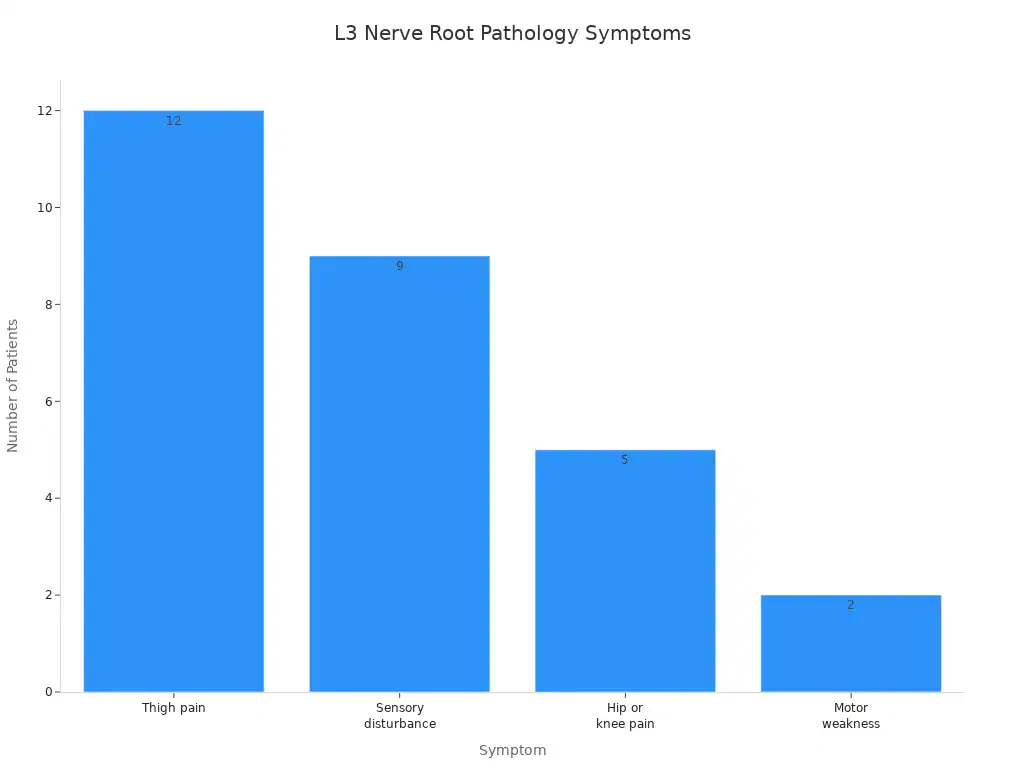
Patients can also show motor deficiencies. These affect the quadriceps femoris muscle. They might have difficulty extending their knee. Sensory alteration often radiates into the mid-thigh and medial knee. This indicates a problem with the L3 nerve. These clinical signs help doctors diagnose conditions like radiculopathy. Radiculopathy occurs when a nerve root becomes compressed or irritated. Assessing the L3 dermatome helps confirm the diagnosis. This allows for targeted treatment. The L3 nerve is crucial for lower limb function.
L4 Lumbar Dermatome: Leg and Foot
L4 Nerve Root
The L4 nerve root originates from the spinal cord at the L4 spinal segment. It forms from both sensory and motor fibers. These fibers combine to create the L4 spinal nerve. This nerve exits the spinal column through the intervertebral foramen between the L4 and L5 vertebrae. The L4 nerve contributes to the lumbar plexus. This network of spinal nerves serves the lower limbs. It plays a significant role in sensation and movement for the leg and foot.
L4 Sensory Distribution
The L4 dermatome covers a distinct area of the lower limb. This dermatome provides sensation to the skin over the lower back. It also includes the front of the thigh and the knee. The L4 dermatome extends down the inner calf and to the inside of the ankle. Specifically, it covers parts of the thigh, knee, leg, and foot. This specific dermatome acts as a key indicator for problems affecting the L4 nerve. Understanding this sensory map helps clinicians identify the precise location of a nerve issue.
L4 Clinical Presentations
Involvement of the L4 nerve can cause various symptoms. Patients often experience pain radiating from the lower back to the front of the thigh. They may also report sensory changes. These changes include numbness or tingling in the anterior thigh and knee. A doctor assesses these symptoms to pinpoint the affected nerve.
Nerve Root | Sensory Distribution | Motor Weakness | Reflex Affected |
|---|---|---|---|
L4 | Anterior thigh and knee | Knee extension, Hip flexion, Hip adduction | Patellar |
Patients can also show motor deficiencies. They might experience weakness in the quadriceps. This weakness affects knee extension. They may also have difficulty with hip flexion and hip adduction. A reduced knee reflex is another common sign of L4 nerve dysfunction. These clinical signs help doctors diagnose conditions like radiculopathy. Radiculopathy occurs when a nerve root becomes compressed or irritated. Assessing the L4 dermatome helps confirm the diagnosis. This allows for targeted treatment.
L5 Lumbar Dermatome: Lateral Leg and Foot
L5 Nerve Root
The L5 nerve root comes from the spinal cord at the L5 spinal segment. It forms from both sensory and motor fibers. These fibers work together. They create the L5 spinal nerve. This nerve exits the spinal column through the intervertebral foramen. This opening is between the L5 and S1 vertebrae. The L5 nerve root has a unique feature. It typically does not split close to its origin. Other lumbar nerves (L1-L4) often do this. The L4 peroneal branch helps locate the L5 nerve. This branch inserts along the side of the L5 nerve. This often happens at the sacrum level. The L5 nerve is also about twice as thick as the L4 peroneal branch at the sacrum.
The L5 nerve’s origin can vary slightly. For people with 23 presacral vertebrae (PSV), the thicker L5 nerve starts from the first sacralized foramen. For those with 24 PSV, the L5 nerve is found along the side of the sacrum. In cases of 25 PSV, the L5 nerve might come from a lumbarized S1. This nerve is a key part of the lumbar plexus. This network of nerves serves the lower limbs. It plays a big role in sensation and movement for the lateral leg and foot.
L5 Sensory Distribution
The L5 dermatome covers a specific area of the lower limb. This dermatome provides sensation to the skin over the lateral leg. It also includes the top of the foot. The L5 dermatome extends to the first, second, and third toes. This means it covers the big toe, the second toe, and the third toe. The L5 lumbar nerve root innervates the skin over the lateral leg and the top of the foot. Understanding this specific sensory map helps doctors. They can identify the exact location of a nerve issue. This dermatome acts as an important sign for problems affecting the L5 spinal nerve. This specific dermatome is one of several dermatomes that map sensation in the lower body.
L5 Clinical Presentations
Problems with the L5 nerve can cause various symptoms. Patients often feel pain that starts in the lower back. This pain can travel down the leg and into the foot. This is a common sign of L5 nerve involvement.
Common clinical signs of L5 nerve root compression include:
Lower Back Pain: This is often the first symptom. It can get worse with movement. Bending or lifting can make it more intense.
Sciatica: This is a distinct type of pain. It goes from the buttock down the thigh. It continues into the lower leg and foot.
Numbness and Tingling: People often describe this as a ‘pins and needles’ feeling. It usually occurs on the top of the foot and in the middle toes.
Weakness: Muscle weakness is common. It especially affects the foot. This can make it hard to lift the front of the foot. This condition is known as foot drop.
Loss of Reflexes: Reflexes in the lower leg might be reduced or missing. This is particularly true around the ankle.
These clinical signs help doctors diagnose conditions like radiculopathy. Radiculopathy happens when a nerve root becomes squeezed or irritated. Assessing the L5 dermatome helps confirm the diagnosis. This allows for specific treatment. The L5 nerve is very important for lower limb function.
Clinical Significance of Lumbar Dermatomes
Understanding lumbar dermatomes is crucial in healthcare. These sensory maps guide clinicians in diagnosing and managing various conditions. They provide a clear picture of nerve function in the lower body.
Diagnosing Radiculopathy and Nerve Compression
A herniated disc in the lumbar spine can press on nerve roots. This compression affects sensation in corresponding lumbar dermatomes. A dermatome is an area of skin. Sensory nerves from a single spinal nerve root supply this area. Dermatome maps show how spinal nerves innervate the skin. Sensory symptoms in a specific dermatome help locate suspected radiculopathy.
Clinicians use dermatome maps as diagnostic tools. They localize nerve damage. However, dermatomal pain patterns can vary.
Nerve Root Level | Dermatomal Pain Pattern | Sensitivity (SE) | Specificity (SP) | Notes |
|---|---|---|---|---|
Lumbar (overall) | Non-dermatomal in <2/3 (64.1%) | Low | Low | |
S1 | 64.9% dermatomal | 0.65 | 0.80 | Most useful dermatomal pattern |
L4 & L5 | Commonly deviated from classic dermatomal pattern | N/A | N/A | Based on nerve root block studies |
Other levels (excluding S1) | Not useful for diagnosis | N/A | N/A | Clinicians should not expect dermatomal pain |
This table shows that while S1 often follows a dermatomal pattern, other lumbar levels, like L4 and L5, can deviate. This means clinicians must consider other factors alongside dermatome assessment when diagnosing radiculopathy.
Spinal Cord Injury Identification
Dermatomes are vital for assessing spinal cord injuries (SCI). The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) examination is the gold standard. This exam systematically checks specific dermatomes and myotomes. It identifies injured spinal cord segments.
Clinicians assess light touch and pinprick sensation across 28 dermatomes (C2 to S4/5) on each side.
Each sensory dermatome receives a score: 0 (absent), 1 (altered), or 2 (normal). They compare this to the individual’s face.
The most caudal intact dermatome (graded as 2) for both light touch and pinprick defines the sensory level.
The neurological level of injury (NLI) is the highest of the sensory and motor levels.
Assessing S4-5 segments helps determine if the injury is complete or incomplete. Sensation or motor function in these segments indicates an incomplete injury.
Here are some key dermatome landmarks:
Dermatome | Body Region |
|---|---|
L1 | Hip girdle and groin |
L2-L3 | Front of thighs |
L4-L5 | Medial and lateral lower leg |
S1 | Heel and middle back of leg |
S4-S5 | Perineal region (including skin at and adjacent to the anus) |
Differentiating Neuropathy
Clinicians often need to distinguish between radiculopathy and peripheral neuropathy. They start by assessing sensory examination findings. They look for sensory signs that match either a peripheral nerve or a dermatomal distribution. This careful approach helps tell the difference.
Condition | Problem Location | Sensory Pattern |
|---|---|---|
Radiculopathy | Nerve root (spine) | Follows a dermatome |
Peripheral Neuropathy | Peripheral nerve level | Follows a cutaneous nerve field |
A dermatome pattern points to a nerve root issue. A cutaneous nerve field pattern suggests a problem with a peripheral nerve. This distinction is critical for accurate diagnosis and treatment.
Practical Clinical Applications
Healthcare professionals use dermatome knowledge daily. This knowledge helps them in many ways.
Neurological Diagnosis and Localization: Clinicians use dermatomes to identify nerve root involvement. This guides treatment decisions. For example, lower back pain with specific dermatomal sensory deficits can indicate a herniated disc. This improves diagnostic speed and treatment accuracy.
Pain Management and Rehabilitation: Dermatome maps help design targeted nerve blocks or electrical stimulation therapies. They identify the exact skin areas supplied by affected nerves. This allows for localized treatments to reduce pain and enhance recovery.
Surgical Planning and Intraoperative Guidance: Surgical teams use dermatomes to prevent nerve damage during procedures. Preoperative mapping helps plan incisions around critical nerve pathways. Intraoperative nerve monitoring correlates with dermatome maps to confirm nerve integrity.
Physiotherapists also rely on dermatomes:
Assessment of Sensation: They test sensation in specific dermatomal areas. This identifies abnormalities like numbness or tingling. It aids in diagnosing conditions such as radiculopathy or peripheral nerve injuries.
Localization of Lesions: Sensory deficits in a particular dermatomal pattern help physiotherapists find the approximate location of a nerve root or spinal cord lesion.
Treatment Planning: Dermatome assessments guide the design of appropriate interventions. A sensory deficit in a specific dermatome due to nerve injury informs the treatment program.
Monitoring Progress: Regular dermatome assessments track patient progress during rehabilitation. They show improvement or the need for treatment adjustments.
Pain Management: Knowledge of dermatomes helps understand referred pain patterns. This allows physiotherapists to tell the difference between musculoskeletal and neurological pain sources. They can then develop appropriate management strategies.
For example, a 60-year-old patient recovered from lumbar spinal surgery. They had reduced sensation in the L4 dermatome. Sensory retraining, neuromuscular re-education, and progressive mobility exercises guided by dermatomal mapping led to marked improvement.