Kidneys play a critical role in maintaining the body’s magnesium balance. While magnesium is essential for many bodily functions, excessive intake poses significant dangers, especially for kidney health. This excess leads to a condition called hypermagnesemia. Approximately 10% of the global population is affected by chronic kidney disease, making careful magnesium regulation even more vital. A population-based study reported an overall prevalence of hypermagnesemia at 3.0%, highlighting its occurrence. Understanding the side effects of magnesium on kidneys is crucial for overall well-being and kidney protection.
Key Takeaways
Too much magnesium in the blood is called hypermagnesemia. This condition can be dangerous, especially for people with kidney problems.
Healthy kidneys remove extra magnesium from the body. Kidneys that do not work well cannot remove magnesium, causing it to build up.
Taking too many magnesium supplements or certain medicines can cause magnesium levels to become too high. This is very risky for people with kidney disease.
High magnesium levels can cause symptoms like weakness, dizziness, and serious heart or brain problems. Seek medical help if you notice these signs.
People with kidney disease should talk to their doctor about magnesium. They should avoid magnesium supplements and products unless a doctor says it is safe.
Hypermagnesemia and Kidney Function

What Is Hypermagnesemia
Hypermagnesemia occurs when a person has too much magnesium in their blood. This condition can become dangerous. Doctors diagnose hypermagnesemia through blood tests.
These tests show high magnesium levels. Normal magnesium levels typically range from 1.7 to 2.3 milligrams per deciliter (mg/dL). A level above 2.6 mg/dL indicates hypermagnesemia. Doctors classify the severity of hypermagnesemia:
Mild: less than 7 mg/dL
Moderate: 7 to 12 mg/dL
Severe: more than 12 mg/dL Additional tests, like a urinalysis, check kidney function. An electrocardiogram (EKG) can detect abnormal heart rhythms.
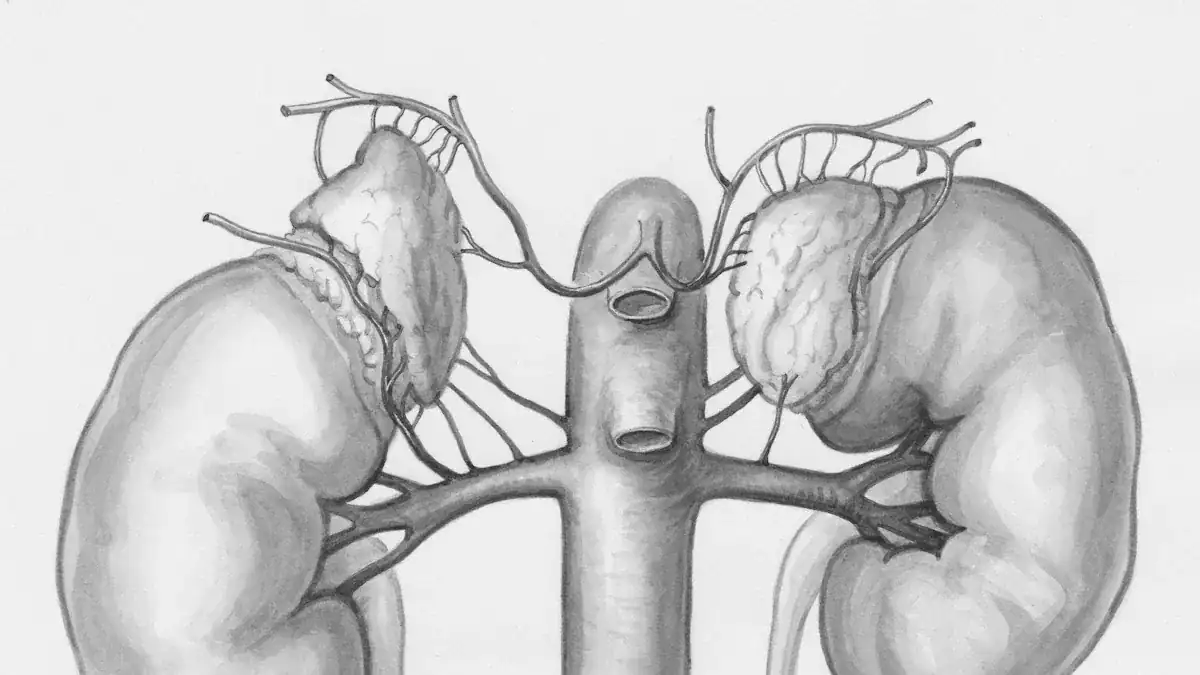
How Kidneys Regulate Magnesium
The kidney plays a crucial role in maintaining proper magnesium levels. Healthy kidneys efficiently eliminate excess magnesium from the body. Approximately 70–80% of the magnesium in plasma is filterable. The kidney tubules reabsorb about 95% of this filtered magnesium.
Only about 5% of the filtered magnesium leaves the body in urine. This process ensures the body maintains a healthy balance. Efficient magnesium excretion generally requires a glomerular filtration rate (GFR) above 20–30 mL/min.
Kidney Impairment and Magnesium Buildup
Poor kidney function directly impairs the body’s ability to excrete magnesium. When the kidneys do not work well, they cannot remove excess magnesium effectively. This leads to a dangerous accumulation of magnesium in the blood. Serum magnesium levels tend to increase when the GFR falls below 20–30 mL/min. This indicates impaired excretion. This buildup causes hypermagnesemia. Individuals with impaired kidney function are at a higher risk for developing hypermagnesemia. This dangerous accumulation can lead to serious health problems.
Causes and Risks of Magnesium Toxicity
Primary Causes of High Magnesium
Several factors can lead to a high magnesium level in the body. The most common non-renal causes of elevated magnesium levels include certain medical conditions. For example, Addison’s disease, where the adrenal glands do not produce enough hormones, can cause magnesium to build up. Hypothyroidism, an underactive thyroid, also contributes to this issue.
Conditions involving rapid cell destruction, such as Tumor Lysis Syndrome during chemotherapy for cancers like Leukemia, Lymphoma, or multiple Myeloma, release cellular components, including magnesium, into the bloodstream. Other causes include hemolysis, which is the destruction of red blood cells, and hypercalcemia, or high calcium levels. Injuries from trauma, shock, or burns can also disrupt magnesium balance. Excessive dietary intake of magnesium, often from certain products, also plays a significant role in developing hypermagnesemia.
Kidney Disease as a Major Risk Factor
Kidney disease stands out as a major risk factor for magnesium toxicity. Healthy kidneys efficiently filter and remove excess magnesium from the body. When kidney function declines, this ability becomes severely impaired.
The kidneys cannot excrete magnesium effectively, leading to its dangerous accumulation in the blood. This makes individuals with any degree of kidney impairment highly susceptible to hypermagnesemia.
The side effects of magnesium on kidneys are particularly severe in these patients because their bodies cannot handle even normal magnesium loads, let alone high doses of magnesium. Therefore, kidney disease significantly increases the risk of developing magnesium toxicity.
Over-Supplementation and Magnesium Products
Taking high doses of magnesium supplements is a significant cause of magnesium toxicity. The Tolerable Upper Intake Level (UL) for magnesium from supplements for adults is 350 milligrams daily. Consuming supplements above this level can lead to side effects such as diarrhea, nausea, and cramping in some individuals. While some evidence suggests higher doses might be safe for certain people, exceeding this UL should only happen under a healthcare provider’s advice.
Many over-the-counter products also contain substantial amounts of magnesium. These include laxatives, antacids, and Epsom salts. Using these products frequently or in large quantities can introduce high doses of magnesium into the body, leading to hypermagnesemia.
Individuals with kidney problems must avoid magnesium supplements and magnesium-containing over-the-counter products due to the high risk of dangerous buildup and severe side effects of magnesium on kidneys.
Medications Affecting Magnesium Levels
Certain medications can also affect magnesium levels in the body, contributing to hypermagnesemia. Lithium-based psychotropic drugs, used to treat mood disorders, can interfere with magnesium excretion. Some medications might also increase magnesium absorption from the gut or reduce its elimination by the kidneys. This can lead to an unwanted accumulation of magnesium, especially when combined with other risk factors or if a person takes high doses of magnesium from other sources. Patients should always discuss all medications and supplements with their doctor to understand potential interactions and risks.
Symptoms of High Magnesium
Early Signs of Hypermagnesemia
High magnesium levels in the blood, known as hypermagnesemia, can present with various signs. Mild hypermagnesemia often shows no symptoms. However, some individuals may experience early signs of magnesium toxicity.
These can include general weakness, feelings of nausea, dizziness, and confusion. Symptoms typically begin to appear when magnesium levels in the blood go above 4–5 mg/dL. It is important to recognize these subtle changes.
Moderate to Severe Symptoms
As magnesium levels continue to rise, the symptoms of hypermagnesemia become more noticeable and serious. Individuals may experience more pronounced muscle weakness and a decrease in reflexes.
They might also feel very tired or drowsy. These moderate symptoms indicate a more significant imbalance in the body’s magnesium levels. Without intervention, the condition can worsen.
Neurological and Cardiovascular Effects
Severe hypermagnesemia significantly impacts the nervous system and heart. Neurological complications can range from altered consciousness, such as drowsiness or coma, to complete paralysis. Some patients may even enter a pseudocomatose state, mimicking a serious brain injury.
Other neurological signs include dysautonomia, severe muscle weakness, and respiratory failure. The cardiovascular system also suffers. High magnesium can impair the heart’s ability to contract and relax properly. This leads to serious issues like arrhythmia, where the heart beats irregularly.
It can also cause myocardial depression, weakening the heart’s pumping action, and vasodilation, which lowers blood pressure. These severe effects increase the risk of mortality.
When to Seek Medical Help
Recognizing when to seek medical help for high magnesium is crucial. Hypermagnesemia can cause severe symptoms when serum magnesium levels are more than 4.8 mg/dL.
Immediate medical attention is necessary if someone shows severe symptoms of hypermagnesemia, especially if they have known kidney problems. Extremely high levels, around 10 mmol/L, can lead to asystole, which is a complete stop of heart activity. Always consult a doctor if you suspect signs of magnesium toxicity or experience any concerning symptoms.
Impact on Kidney Disease Patients
Patients with kidney disease face unique challenges with magnesium balance. Their impaired kidney function makes them especially vulnerable to the side effects of magnesium on kidneys. This section explores how high magnesium levels affect individuals with compromised kidney health.
Magnesium and End-Stage Renal Disease
End-stage renal disease (ESRD), also known as kidney failure, severely impacts the body’s ability to manage magnesium. When kidneys fail, they cannot effectively remove excess magnesium from the blood. This leads to hypermagnesemia. A study looked at 101 hemodialysis patients. It found that 16.8% of these patients had hypermagnesemia (serum magnesium >1.5 mmol/L). No patients had severe hypermagnesemia (>2.0 mmol/L). The average serum magnesium concentration was 1.32 ± 0.18 mmol/L.
Metric | Value |
|---|---|
Patients screened | 101 |
Prevalence of hypermagnesemia (>1.5 mmol/L) | 16.8% (17 patients) |
Prevalence of severe hypermagnesemia (>2.0 mmol/L) | 0% (no cases) |
Mean serum magnesium concentration | 1.32 ± 0.18 mmol/L |
High magnesium levels in ESRD can also affect parathyroid hormone (PTH) secretion. PTH helps regulate calcium and phosphorus in the body. A study of 110 hemodialysis patients found that higher serum magnesium levels correlated with lower PTH levels.
This inverse relationship remained even after accounting for calcium and phosphorus. Patients with very low PTH levels had significantly higher serum magnesium concentrations (3.01 ± 0.33 mg/dL) compared to those with higher PTH levels (2.63 ± 0.38 mg/dL).
This suggests that chronic hypermagnesemia may reduce PTH production or release in patients with kidney failure. This suppression of PTH can contribute to hypocalcemia, a condition where the body has too little calcium.
Effects on Bone Metabolism
Too much magnesium can have adverse effects on bone metabolism in chronic kidney disease (CKD) patients. The delicate balance of minerals is crucial for healthy bones. When magnesium levels are too high, it can interfere with this balance.
As mentioned, high magnesium level can suppress PTH. PTH plays a vital role in bone health. Its suppression can lead to problems with bone turnover and mineralization. This makes bones weaker and more prone to issues in patients already struggling with kidney failure.
Vascular Calcification Concerns
Vascular calcification is a serious problem for CKD patients. It involves the hardening of blood vessels. This increases the risk of heart disease. Magnesium plays a complex role in this process. In laboratory studies, magnesium shows several protective effects against vascular calcification:
It stops the formation of hydroxyapatite crystals. These crystals are key for bone-like changes in blood vessel cells.
It affects the maturation of calciprotein particles. These particles also cause bone-like changes in blood vessel cells.
It reduces the expression of genes that promote bone formation. It also prevents the loss of substances that stop calcification.
Magnesium uptake through specific channels (TRPM7) blocks a signaling pathway (Wnt/β-catenin). This pathway regulates bone-like changes in blood vessel cells.
It activates a calcium-sensing receptor (CaSR). This reduces bone-like changes in blood vessel cells caused by high phosphate.
It counteracts changes in specific microRNAs caused by high phosphate levels.
However, clinical trials show mixed results. One study in Japan gave oral magnesium oxide to CKD patients. They saw a significantly smaller increase in vascular calcification compared to a control group. Another study in Denmark/Norway gave oral magnesium hydroxide. This study found no difference in calcification progression between the treatment and placebo groups, even though magnesium levels increased.
A meta-analysis combined results from several studies. It found that magnesium supplementation increased serum magnesium levels and reduced calcium, PTH, and carotid intima-media thickness. However, it did not reduce vascular calcification scores in CKD patients. More research with larger groups of patients is needed to fully understand magnesium’s effect on vascular calcification.
Preventing Magnesium Overload
Preventing magnesium overload is crucial, especially for individuals with compromised kidney function. People can take several steps to maintain healthy magnesium levels. These steps help avoid the dangerous condition of hypermagnesemia.
Safe Magnesium Supplementation
Individuals should approach magnesium supplementation with caution. Always check the dosage on supplement labels.
Dietary Considerations for Kidney Health
Diet plays a significant role in managing magnesium intake. Many foods naturally contain magnesium. These include leafy green vegetables, nuts, seeds, and whole grains. For most healthy individuals, dietary magnesium does not pose a risk of overload.
However, people with kidney disease must be careful. They should discuss their diet with a dietitian or doctor. These professionals can help create a meal plan that balances nutrient needs while preventing mineral buildup.
Monitoring for At-Risk Individuals
Regular monitoring is essential for individuals at risk of magnesium overload. This group includes people with kidney impairment or those taking magnesium-containing medications.
Doctors can perform blood tests to check magnesium levels. These tests help detect rising levels before symptoms appear. Individuals should also pay attention to their bodies. They should report any early signs of hypermagnesemia to their doctor.
Consulting Healthcare Professionals
Consulting healthcare professionals is the most important step in preventing magnesium overload. A doctor can assess individual risk factors. They can also provide personalized guidance on supplementation and diet. This is especially true for patients with existing kidney conditions. Regular check-ups and open communication with medical staff ensure safe management of magnesium levels.
Maintaining the right balance of magnesium intake is crucial, especially for kidney health. The side effects of magnesium on kidneys can be severe when levels become too high. Hypermagnesemia poses a particular threat to compromised kidneys.
It can cause adverse neuromuscular effects, muscle defects, and serious cardiovascular problems like reduced heart rates. Healthy individuals usually filter excess magnesium from food effectively. However, those with impaired kidney function must avoid magnesium supplements. This prevents toxic levels. Individuals should take proactive steps. These include careful supplementation and dietary awareness. Always consult healthcare professionals for ongoing medical consultation and monitoring. This is vital for those with kidney concerns to prevent serious complications.

