Posterior tibial tendonitis affects a crucial tendon in your foot. This posterior tibial tendon acts as the main tendon that supports the arch of your foot. When this tendon experiences inflammation, it can lead to dysfunction.
This may cause your foot arch to collapse, a condition known as adult-acquired flatfoot. Recognizing early symptoms is key for better outcomes. Many cases of this tendonitis go undiagnosed.
For example, 3.3% of women over 40 had undiagnosed symptomatic Stage I and II posterior tibial tendonitis in one study. Around 10% of older women experience this tendonitis. Understanding these symptoms helps you manage this condition effectively.
Key Takeaways
Posterior tibial tendonitis is when a key foot tendon gets inflamed. This tendon supports your arch. Early signs are important to notice.
Symptoms include pain on the inside of your ankle, swelling, and changes in your foot’s arch. Your foot might flatten over time.
Rest, ice, and special shoe inserts (orthotics) can help. Physical therapy exercises strengthen your foot and ankle.
If not treated, the condition can get worse. It can lead to a flatfoot deformity. Surgery might be needed in severe cases.
Prevent recurrence by strengthening your foot, wearing good shoes, and managing your weight. Listen to your body and avoid activities that cause pain.
Understanding Posterior Tibial Tendonitis
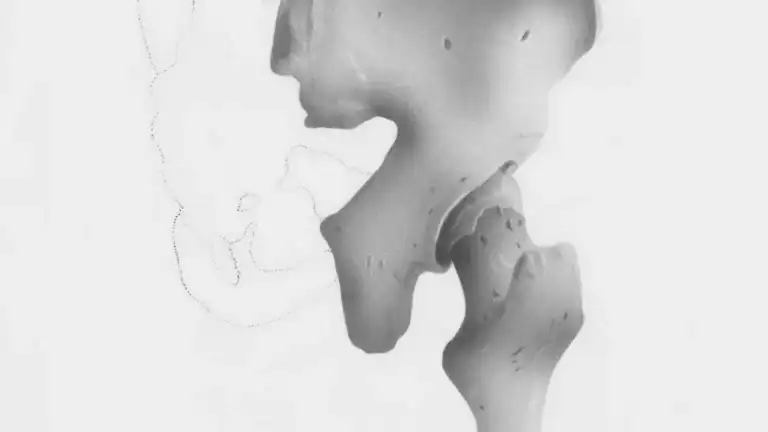
The Posterior Tibial Tendon’s Role
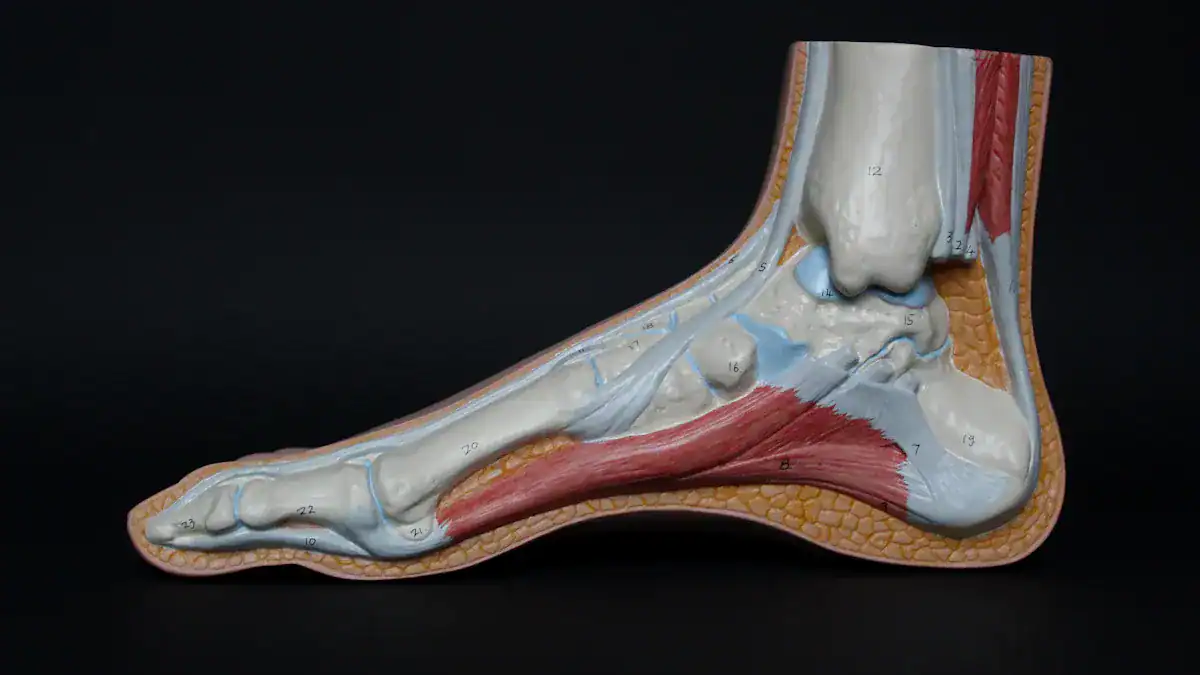
You have a crucial structure in your foot called the posterior tibial tendon. This tendon does more than just connect muscle to bone. It actively stabilizes your hindfoot. It also helps control how your midfoot moves when you walk.
When you stand, this posterior tibial tendon works to keep your arch from collapsing. It pulls parts of your foot together, creating strong support. This action makes your foot rigid for pushing off the ground. The posterior tibial tendon is the main dynamic stabilizer of your medial longitudinal arch. It helps your foot become a strong lever for movement. Without a healthy posterior tibial tendon, your foot loses its structural integrity.
How Tendonitis Develops
Posterior tibial tendonitis happens when this important posterior tibial tendon becomes inflamed. This inflammation often results from overuse or repetitive stress. Think of it as an injury from too much strain.
Any direct injury to the tendon can also cause it. Sometimes, the tendon does not just get inflamed. It can also undergo degenerative changes. This condition is called tendinosis. Tendinosis involves tiny tears and a breakdown of the tendon’s collagen. It does not always involve inflammation.
Both tendonitis and tendinosis can weaken the posterior tibial tendon. This makes your foot less stable. Chronic tendinosis often develops from prolonged stress. This type of tendinosis requires careful management.
Progression to Dysfunction
If you do not address posterior tibial tendonitis, it can worsen. This progression leads to posterior tibial tendon dysfunction. The condition moves through several stages:
Stage 1: You experience mild tendonitis or inflammation around the posterior tibial tendon. Your foot structure remains normal. You can still raise your heel, but it might hurt.
Stage 2: You cannot raise your heel. Your arch starts to collapse, but it is still flexible. Your toes might begin to point outward. This is a sign of posterior tibial tendon dysfunction.
Stage 3: Your arch has collapsed and become rigid. Your toes and heel turn outward. You may see signs of arthritis in your subtalar joint. This indicates significant posterior tibial tendon dysfunction.
Stage 4: All previous symptoms are present. X-rays show displacement in your ankle. You might also have ankle joint arthritis. This is the most severe stage of posterior tibial tendon dysfunction.
This progression shows how initial inflammation can lead to serious foot deformity and pain. Early intervention is key to prevent severe tendinosis and dysfunction of the posterior tibial tendon. Untreated tendinosis can lead to irreversible changes.
Identifying Posterior Tibial Tendonitis Symptoms

Recognizing the symptoms of posterior tibial tendonitis early helps you get treatment faster. You can prevent the condition from getting worse. Pay close attention to changes in your foot and ankle. These changes can signal a problem with your posterior tibial tendon.
Early Signs of Tendonitis
You might first notice subtle signs of posterior tibial tendonitis. These early symptoms often appear after you increase your activity level. You may feel a dull ache or discomfort.
In tibialis posterior tendinosis, early on people have occasional pain behind the inner ankle with increased activity.
This pain might come and go. You might not think much of it at first. However, this early pain is your body telling you something is wrong. Do not ignore these initial warning signs.
Pain Location and Characteristics
The pain from posterior tibial tendonitis usually focuses on the inside of your ankle and foot. You might feel it along the path of the posterior tibial tendon. This pain can be sharp or a dull ache. It often gets worse with activity. You might notice pain in specific areas:
The back and bottom of your ankle.
The area extending into your medial malleolus (the bony bump on the inside of your ankle).
The medial navicular (a bone on the inside of your foot). You can feel pain if someone presses on it.
The medial aspect of the posterior tibia (the inner part of your shin bone). You feel pain when someone touches this area.
You may also feel pain around the navicular tuberosity. This is a bony bump on the inside of your foot. The area behind the medial malleolus often shows where the tendon degenerates. Swelling here is a key sign. Irritation can also occur where the tendon and the posterior medial malleolus touch.
Swelling, Tenderness, and Stiffness
You will likely experience swelling and tenderness along the posterior tibial tendon. This swelling often appears on the inside of your ankle. The area will feel sore when you touch it. The presence of swelling and tenderness can also tell you about the severity of your condition.
Stage | Diagnostic Features Related to Swelling and Tenderness |
|---|---|
1 | Pain and swelling of the tendon are present, but you can still perform a single-leg heel raise. There is no foot deformity. |
2 | Pain and swelling of the tendon persist, but you cannot perform a single-leg heel raise. Foot deformities like pes planus and midfoot abduction appear. |
3 | All features of Stage 2 are present. You also have a fixed subtalar joint and arthritis. |
Pain and swelling with tenderness of the tibialis posterior tendon behind the medial malleolus indicate tenosynovitis. In cases of tenosynovitis, the pain is typically more acute. The tendon may feel thick and swollen.
If you have unilateral arch collapse, medial ankle bulging, and forefoot abduction, along with pain and swelling with tenderness, this suggests advanced tendon pathology. You need testing for tendon rupture.
This means that while swelling and tenderness are present, their association with other severe symptoms points to increased severity. You might also notice pain and stiffness in your foot, especially in the morning or after rest.
Arch Changes and Foot Deformity
One of the most noticeable symptoms of posterior tibial tendonitis is a change in your foot’s arch. As the tendon weakens, it can no longer support your arch effectively. This leads to a gradual flattening of your foot.
Posterior tibial tendon dysfunction is the most common cause of adult-acquired flatfoot deformity.
In Stage II, your foot becomes deformed. By Stage III, the foot is significantly deformed.
A ‘flat foot’ means your foot’s arch lies flat on the inner side, and your foot points outwards.
Advanced posterior tibial tendon dysfunction can result in a rigid adult acquired flatfoot deformity.
You might notice your arch collapsing. Your toes may start to point outward. This change in foot shape can become permanent if you do not treat it. These are clear symptoms of posterior tibial tendonitis progressing.
Functional Limitations
Posterior tibial tendonitis can severely limit your daily activities. The pain and weakness make many movements difficult. You might find it hard to do things you once enjoyed. Common activities that become challenging include:
Running
Walking for a long time
Standing for a long time
Playing sports like basketball, tennis, or soccer
Basic movement, such as walking or standing
Running, especially on hills
These functional limitations are important symptoms. They show how much the condition affects your quality of life. Recognizing these limitations helps you understand the impact of posterior tibial tendonitis.
Causes and Risk Factors
Understanding the causes of posterior tibial tendonitis helps you prevent this condition. Several factors can contribute to the strain and inflammation of your posterior tibial tendon. You can identify your risks by knowing these factors.
Common Causes of Tendon Strain
Your posterior tibial tendon can experience strain from various activities. Acute injury, like a fall, can directly damage the tendon. Overuse is another frequent cause. Repetitive use in high-impact sports, such as basketball, tennis, or soccer, often leads to problems.
Repetitive stress from daily activities also contributes. Small injuries to the tendon can occur from a sudden increase in your activity level. These factors put stress on your foot.
Anatomical Predispositions
Certain features of your foot can make you more prone to posterior tibial tendonitis. If you have flatfoot, your arch provides less support. This puts extra stress on the posterior tibial tendon.
Foot structure abnormalities, whether you were born with them or developed them later, also increase your risk. These structural issues change how your foot bears weight.
Lifestyle and Activity Risks
Your daily activities and lifestyle choices impact your tendon health. Runners often develop this condition due to repetitive motion. Activities involving prolonged standing or excessive walking also increase risk.
Dancers and gymnasts face higher risks because of their demanding movements. If you have a highly active lifestyle, you put more stress on your feet. High-impact sports like basketball, tennis, or soccer also contribute to tendon injury.
Age and Gender Influence
Age and gender play a role in who develops posterior tibial tendonitis. Obese, middle-aged women show a 10% prevalence of posterior tibialis tendon dysfunction. One study found a 3.3% prevalence of posterior tibial tendon tear in women over 40 years of age.
Most studies on this condition include patients with a mean age over 40 years. However, younger individuals, specifically those aged 18 to 25 years with flatfeet, can also experience this problem. A study showed an 18.54% prevalence in this younger group.
Diagnosing Posterior Tibial Tendonitis
You need an accurate diagnosis to start proper treatment for posterior tibial tendonitis. Doctors use several methods to understand your condition. This process helps confirm the problem and rule out other issues.
Clinical Examination
Your doctor begins with a thorough physical examination. They observe the shape and functionality of your foot. They look for a collapsed arch. You might find it difficult to rise onto your tiptoes while standing on one leg.
The doctor also performs manual tests. They press on the tendon to check for tenderness. They move your foot in specific ways to identify pain and how your tendon responds. You will likely feel tenderness over the inside ankle and foot. The doctor assesses any difficulty you have with a tip-toe walk or a single heel-rise. This initial examination provides crucial information for your diagnosis.
Imaging for Confirmation
Doctors often use imaging tests to confirm a diagnosis and assess severity. Magnetic Resonance Imaging (MRI) is the preferred tool. It offers superior accuracy, sensitivity, and specificity.
Modality | Sensitivity | Specificity | Accuracy (for PTT tears) |
|---|---|---|---|
MRI | Up to 95% | Up to 100% | 96% |
Ultrasound (tendinopathy) | 80% | 90% | N/A |
Ultrasound (peritendinosis) | 90% | 80% | N/A |
Radiography (PTT ruptures) | 71.4% | 88.9% | 81.3% |
While ultrasound and radiography can provide an initial assessment, MRI gives a definitive diagnosis. It helps your doctor see the extent of any tendon damage in your foot.
Ruling Out Other Conditions
Sometimes, other conditions can mimic posterior tibial tendonitis. Your doctor must rule these out to ensure you receive the correct treatment. For example, peroneal tendinopathy and tibialis anterior tendinopathy can present with similar symptoms.
Other tendon injuries around the ankle can also be mistaken for posterior tibial tendonitis. Your doctor will specifically screen for these conditions. This careful differentiation ensures your diagnosis is precise.
Immediate Relief Strategies
When you first feel symptoms of posterior tibial tendonitis, immediate steps can help. These actions focus on reducing pain and inflammation. They also protect your tendon from further damage. Starting these strategies early supports your overall rest and recovery.
Rest and Activity Modification
Giving your foot proper rest is the most important step. This initial rest is vital for healing. You need to modify your activities to reduce stress on the tendon. This period of rest and recovery helps prevent further damage. You should use crutches or a walking boot.
These devices lessen pressure on your inflamed tendon. Avoid high-impact activities like running or jumping. These activities stress the tendon. Limit long periods of standing or walking. Consider using a walker or cane if moving is difficult. Elevate your affected foot.
This reduces swelling by helping fluid drain. Orthotic supports or shoes with good arch support also relieve tendon strain. This comprehensive rest allows your body to begin the healing process. Patience and compliance with this rest are key for effective rest and recovery. Your body needs this dedicated rest to start mending.
Icing the Affected Area
Applying ice to the affected area helps reduce inflammation and pain. This simple step provides quick relief. Use ice packs or cold packs. Apply them for up to 20 minutes at a time.
Do this several times a day during the initial days. Cold compression helps calm the irritated tendon. It is an important part of your immediate rest and recovery plan. Continue this icing routine as needed. It supports your overall rest and recovery.
Treatment for Posterior Tibial Tendonitis

The treatment of posterior tibial tendonitis varies greatly. It depends on how severe your condition is. You will find that early stages often respond well to conservative treatments. More severe cases might need additional, more intensive treatments. Your doctor will help you decide the best path.
Conservative Treatment Options
You can often manage early-stage posterior tibial tendonitis without surgery. These conservative approaches focus on reducing pain and inflammation. They also aim to support your foot.
Activity Modification: You should stop activities that make your tendon worse. This includes running or sports with sharp movements.
Pain and Inflammation Management: You can apply ice to the affected area. Taking non-steroidal anti-inflammatory drugs (NSAIDs) also helps.
Immobilization: Your doctor might recommend a short leg cast or a walking boot. You wear this for a few weeks to rest the tendon.
Long-term Support: Orthotics (shoe inserts) and braces offer good longer-term support.
Rehabilitation: You will benefit from physical therapy to strengthen the tendon. Both orthotics and physiotherapy are effective for early stages of posterior tibial tendon dysfunction (PTTD). Specific orthotics like the University of California Biomechanics Laboratory foot orthosis, solid ankle foot orthosis (AFO), and the Arizona AFO brace have shown success.
Orthotics and Arch Support
Orthotics play a crucial role in the treatment of posterior tibial tendonitis. They provide essential support for your foot arch. This support helps decrease the load on your posterior tibial tendon. Remember, this tendon acts as the main support for your arches. Orthopedic doctors often recommend custom orthotics. These can be complete customized shoes or shoe inserts. They give total support for your foot arch.
Research shows that foot orthoses with personalized internal longitudinal arch support are more effective. They reduce pain better than flat insoles or standard treatments. These orthotics optimize foot loading. They support and maintain your arch. They also improve foot biomechanics. Success rates can reach up to 90%.
You have several options for orthotics:
Sense Modular Insoles: These come with a standard shell, a medial wedge, and a Kirby Skive. The wedge extends into the arch for increased supination resistance.
Slimline Arch Support Insoles: These feature an increased heel cup. They allow for added wedging. They provide good support and supination resistance.
Heel Plateau Insoles: You get maximum stability and optimal comfort with these. They have an extended support surface and an integrated rolling edge. This reduces pronation speed.
Football Insoles: These are for narrow sports boots. You can adapt them with wedging to increase forces and provide support in athletic footwear.
SOLE footbeds: These are custom moldable orthotics. They offer arch support and a deep heel cup. They are clinically proven to reduce strain in your feet by an average of 34%. They do this by supporting the arch from beneath and promoting neutral alignment.
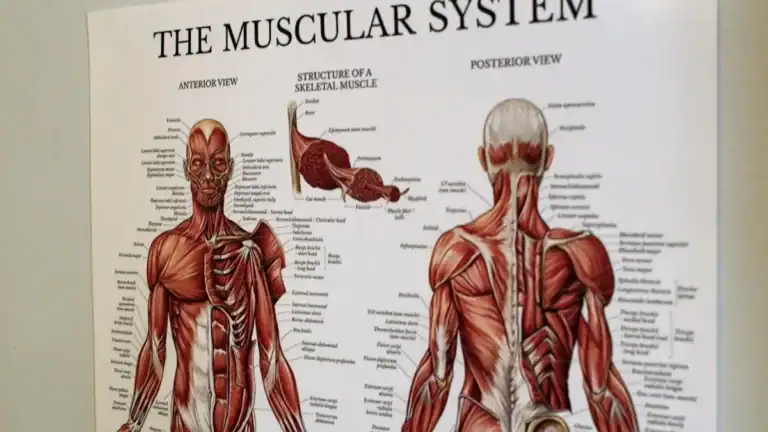
Physical Therapy & Exercises
Physical therapy is a cornerstone of management and treatment for posterior tibial tendonitis. It helps strengthen your tendon and surrounding muscles. Your therapist will guide you through specific exercises for posterior tibial tendonitis.
Unresisted Ankle Movement Through Range: You perform non-weight bearing exercises. These develop strength and pain-free range of motion. They focus on inversion and eversion.
Resisted Movement Through Range: You use resistance bands to build strength. These stimulate healing, focusing on eccentric strength.
Weight Bearing Proprioception: You do barefoot exercises. These dynamically maintain your medial arch height.
Dynamic Weight Bearing Proprioception: You add upper body movement in single-limb stance. This further challenges your tibialis posterior.
Heel Raise with Inversion: This is a weight-bearing exercise. It builds strength in your tibialis posterior and surrounding ankle muscles.
Other beneficial exercises include:
Graded Resistance: While sitting, you use a resistance band. Point your foot downwards and inwards slowly. Start with 8 repetitions, 2 sets. Gradually increase to 3 sets of 10-15 reps with increased resistance. Each repetition should take about 5 seconds.
Balance: You start with single-foot balance for a few seconds. Then, you can close your eyes or stand on a pillow. Progress to reaching out of your base of support for 2 sets of 10-15 reps.
Progressive Loading: These are functional exercises. They support your medial arch during the ‘toe off’ phase of gait.
Seated heel raise: You use weight over your knee (a dumbbell or bag). Do 3 sets of 15 repetitions. Focus on slow lowering (eccentric work).
Two-feet heel raise: Squeeze a ball between your heels. Distribute weight 50:50 initially, then adjust. Focus on slow ascent and even slower descent.
Single-leg heel raise: Perform this on your affected foot. Do this once you can do the two-feet version with 80-90% weight on the affected foot.
Ankle stretches: These improve range of motion and reduce pressure on the tendon.
Ankle strengthening exercises: These improve muscle balance. They prevent overstressing your posterior tibial tendon.
Hip and knee strengthening exercises: These correct alignment issues that might stress the tendon.
Balance and proprioception exercises: These improve foot and ankle function.
Gait training: This is for individuals with difficulty walking or running.
Plyometric exercises: In later stages, these improve load tolerance, especially for athletes.
Surgical Treatment Options
Sometimes, conservative treatments do not work. In these cases, surgery might be necessary. There are several types of surgery to address posterior tibial tendonitis and its complications.
Tenosynovectomy: This surgery removes inflamed tissue lining the tendon.
Tendon Transfer: This surgery replaces the damaged tendon with another foot tendon.
Arthrodesis: This surgery realigns and fuses bones in cases of arthritis.
Osteotomy: This surgery involves cutting heel and midfoot bones to recreate the arch.
Kidner Procedure: This surgery removes an accessory navicular bone if it causes pain.
When Surgery is Considered
You might consider surgery if your symptoms persist or worsen. Your doctor will evaluate several factors.
Posterior tibialis tendon dysfunction: If the tendon is significantly dysfunctional.
Flatfoot: If you have a severe flatfoot deformity, also known as “fallen arches” or Pes planus.
Posterior tibialis tendon injury or rupture: If the tendon is injured or torn.
Symptoms lasting for more than 6 months: If non-surgical treatments have not provided relief over a long period.
Significant loss of function and weakness in the foot: If your daily activities are severely limited.
Desire to return to sports soon: Athletes might opt for surgery to speed up recovery.
Failure of non-surgical treatments to alleviate symptoms: This is a primary indicator that surgery may be needed.
Recovery from Posterior Tibial Tendonitis
You need patience for recovery from posterior tibial tendonitis. Posterior tibial tendon dysfunction typically takes 6-8 weeks to show improvement. Complete relief and full recovery can take up to six months. This requires a dedicated program. You must avoid early activity on a healing tendon. This prevents setbacks in your recovery.
Short-Term Recovery Goals
Your immediate goals focus on reducing pain and protecting the tendon. You should prioritize rest. This allows the inflamed tendon to begin healing. You might use crutches or a walking boot. These devices reduce stress on your foot. Following your doctor’s initial instructions is crucial. This sets the stage for a successful recovery.
Long-Term Rehabilitation Phases
Long-term rehabilitation for posterior tibial tendon dysfunction follows distinct phases. You will progress through these steps.
Initial Immobilization: Your foot is typically immobilized. You might wear a cast or walking boot for several weeks. This protects the healing tendon.
Gradual Weight-Bearing: You slowly reintroduce weight-bearing. Medical guidance is important here. You might use crutches or other aids.
Physical Therapy Initiation: You begin gentle range-of-motion exercises. This helps restore flexibility.
Progressive Strengthening and Balance Training: Exercises advance. You strengthen the tendon and improve balance. This builds resilience.
Long-Term Management: This phase includes supportive footwear. You also gradually return to activities. This ensures optimal long-term outcomes and prevents re-injury.
Factors Affecting Recovery Time
Several factors influence your recovery time for posterior tibial tendonitis. The severity of the damage can prolong recovery time. It might extend to months. Early activity on a regenerating tendon can cause a setback in recovery. Noncompliance with recommended treatment might also cause a setback. You must follow your treatment plan. This helps ensure a smooth recovery.
Safe Return to Activities
You must return to activities safely. Do not rush this process. Your physical therapist will guide you. They help you gradually increase your activity level. This prevents re-injury. Listen to your body. Any new pain means you need more rest. A gradual return ensures lasting recovery.
Preventing Recurrence
You can take proactive steps to prevent posterior tibial tendonitis from returning. This involves a combination of strengthening, proper support, and mindful activity. Prevention is key to long-term foot health.
Strengthening and Flexibility
Strengthening your muscles and improving flexibility are crucial for prevention. You should focus on exercises that support your posterior tibial tendon.
Strengthening Exercises:
Forward Step Downs: This exercise strengthens your quad and soleus muscles. A strong soleus reduces the load on your posterior tibial tendon. Strong quads help maintain proper lower leg positioning.
Seated Soleus Raise with Weight: This specifically challenges your soleus muscle. Consistent repetitions support your posterior tibial tendon.
Flexibility Exercises:
Hamstring wall stretch: Lie on your back with one leg up a wall. Hold for at least 1 minute. Repeat 2-4 times.
Calf wall stretch: Stand facing a wall. Place one leg behind the other. Keep your heel on the floor. Bend your front knee to stretch the calf of your back leg. Hold for up to 30 seconds. Repeat 2-4 times.
Shin muscle stretch: Sit and point your toes downwards. Feel a stretch in the front of your shin. Hold for 15-30 seconds. Repeat 2-4 times.
Ankle inversion with resistance band: Sit with a straight back. Place your affected foot’s outer edge on your other knee. Use a resistance band around the ball of your foot. Slowly invert your foot. Repeat 3-10 times.
Proper Footwear and Support
Choosing the right footwear and using proper support significantly reduces strain on your posterior tibial tendon.
Stability shoes: These shoes have technology to support your foot arches. They control pronation, often on the inner part of the shoe.
Medial support technologies: Look for features like medial posts (harder foam), medial sidewalls, or plastic cages. These add stiffness and support.
Higher drop shoes: These shoes are beneficial because your posterior tibial tendon is a plantarflexor muscle. A higher drop reduces stress on the muscle and tendon.
Orthotics: Custom orthotics with proper posting support your rear foot and arch. They reduce strain on the posterior tibial tendon. They also prevent excessive stretching. Both orthotics and shoes should offer good cushioning and shock absorption. Adequate arch support reduces the workload on your posterior tibial tendon. A deep heel cup prevents excessive heel movement. This ensures a stable base for your foot.
Gradual Activity Progression
You must return to activities slowly. This prevents re-injury. Rehabilitation programs for posterior tibial tendon injuries typically last 10 to 16 weeks. This includes an initial rest period. You should perform exercises daily for at least three months.
Functional Exercises:
Single-leg heel raises: Start with a few. Gradually increase to 50. Lower slowly and with control. Wear shoes and orthotics.
Toe walking: Begin with 8-10 yards. Progress to 100 yards. Keep your heels high off the ground.
Balance board training with tapping: Stand on your affected leg on a balance board. Tap the board to the ground. Return to a balanced position 20 times for each of five directions. Repeat in the opposite direction.
For all rehabilitation exercises with this injury, you should stop if you cause any significant pain. Unlike some other tendon injuries, pushing into pain is not a good idea here!
Weight Management and BMI
Managing your weight is crucial for preventing recurrence. Excess weight places additional stress on your feet and ankles. This increases the likelihood of developing the condition. Studies show that losing even 25 pounds can reduce pain by 30%. Maintaining a healthy weight significantly alleviates strain on your posterior tibial tendon.