
Prostate-specific antigen (PSA) is a protein your prostate gland produces. Doctors use the PSA test as a key tool for prostate health screening. You might wonder, “What are normal PSA levels?” The answer often depends on your age. For example, prostate cancer is a major global health issue; in 2021, the world saw 1.32 million new cases. This prostate health guide helps you understand PSA levels by age and what these results mean for your prostate.
Key Takeaways
PSA is a protein from your prostate gland. Doctors use a PSA test to check prostate health.
Your normal PSA level changes with age. For example, men under 60 usually have levels at or below 2.5 ng/mL.
Many things can raise your PSA levels. These include an enlarged prostate, infection, or even recent activities.
A high PSA level needs more checks. It does not always mean cancer. Your doctor will help you understand the results.
Talk to your doctor about PSA screening. They will help you decide when and how often to get tested.
Understanding PSA
What is PSA?
Prostate-specific antigen, or PSA, is a protein your prostate gland makes. Think of it as a special marker from your prostate. Biochemically, PSA is a neutral serine protease. This means it is an enzyme that breaks down other proteins. It acts much like enzymes involved in blood clotting. Your prostate tissue exclusively produces this glycoprotein. Both normal and cancerous prostate cells create PSA. You find it mainly in semen, but small amounts also appear in your blood. A key job for PSA is splitting seminal vesicle proteins, like semenogelin I and II. This action helps liquefy the seminal coagulum.
Why PSA Matters for Prostate Health
PSA plays a crucial role in male fertility. In the ejaculate, PSA liquefies semen. This allows sperm to swim freely. It also helps dissolve cervical mucus, making it easier for sperm to enter the uterus. This serine protease, also known as kallikrein 3/KLK3, degrades semenogelins I and II. This process is vital for the seminal coagulum to become liquid. Without enough PSA, sperm might not fertilize an egg effectively.
Because your prostate produces PSA, doctors use blood tests to measure its levels. Changes in these levels can signal issues with your prostate. For example, higher PSA levels might suggest an enlarged prostate, inflammation, or even prostate cancer. Understanding your PSA levels helps you and your doctor monitor your prostate health.
PSA Levels By Age Chart
Your PSA levels naturally change as you get older. Doctors use age-specific PSA ranges to understand your prostate health better. What is a normal PSA level by age? This question has different answers depending on your age. You need to know your age-specific PSA range.
Typical PSA Ranges
A single “normal psa level” does not apply to everyone. Your age plays a big role. For men aged 59 or younger, your PSA levels should be at or below 2.5 ng/mL. If you are 60 or older, your PSA levels should be at or below 4.0 ng/mL. Generally, low-risk or normal PSA results are less than 2.0 ng/mL.
For men aged 40-49, the established age-specific PSA range is 0-2.5 ng/mL. The median PSA level for men in this age group is 0.7 ng/mL. A PSA level above 2.5 ng/mL for men aged 40-49 is above the age-specific norm. This may need medical attention. A baseline PSA level between 0.7 ng/mL and 2.5 ng/mL in your 40s increases your risk of prostate cancer by 14.6 times later on.
Historically, the upper limit for PSA was 4.0 ng/mL. However, doctors now recommend a reduction to 2.5–3 ng/mL for patients between 60 and 65 years of age. This table shows a typical PSA range by age:
Age Group | Normal PSA Level (ng/mL) |
|---|---|
40-49 | 0-2.5 |
50-59 | ≤ 2.5 |
60 or older | ≤ 4.0 |
Factors Affecting PSA
Many things can affect your PSA levels. These factors can cause elevated PSA levels even without cancer. You should discuss these with your doctor before your test.
Medical Conditions:
Prostatitis: Inflammation of your prostate gland can increase your PSA.
Benign Prostatic Hyperplasia (BPH): An enlarged prostate, common as you age, can lead to increased PSA production.
Urinary Tract Infection (UTI): An infection near your prostate can raise your PSA levels.
High Parathyroid Hormone (PTH): High levels of PTH may escalate your PSA levels.
Procedures and Activities:
Digital Rectal Exam (DRE): Manipulation of your prostate during this exam can temporarily elevate your PSA.
Ejaculation: This causes minor trauma to your prostate, releasing PSA. Avoid ejaculation for about two days before a PSA test.
Recent Trauma: Injury to your perineal area or groin can temporarily spike your PSA levels.
Cycling: Some studies suggest cycling may contribute to elevated PSA levels.
Urologic Procedures: Procedures like a prostate biopsy, cystoscopy, or colonoscopy can temporarily raise your PSA levels.
Medications:
5-alpha reductase inhibitors (5-ARIs): Medications like finasteride and dutasteride, used for BPH, can artificially lower your PSA results by as much as 50%.
Testosterone Supplements: Over-the-counter libido drugs or testosterone supplements can increase your PSA.
NSAIDs: Medications like ibuprofen can skew your PSA test results.
Statins: Drugs like Lipitor can also skew your PSA test results.
Blood Pressure Medication: Thiazide diuretics may lower your PSA levels.
Erectile Dysfunction Medication: Tamsulosin reduces your PSA levels.
Other Factors:
Age: Your PSA levels naturally increase as you get older.
COVID Infection/Vaccine: A COVID infection can elevate your PSA levels due to inflammation. The COVID vaccine may have a similar effect.
When PSA Levels Are Concerning
A PSA level above 4.0 ng/mL in any age group requires investigation. For men younger than 60, a PSA level above 2.5 ng/mL typically prompts additional testing. Historically, a PSA level greater than 4 ng/mL was a common threshold for recommending a prostate biopsy. However, some studies now use a threshold of 2.5 ng/mL or 3 ng/mL.
Levels between 2.0 and 10.0 ng/mL are considered a ‘gray zone’. Within this range, the Free/Total PSA ratio helps determine your risk of prostate cancer. A dangerously high PSA level is usually above 10.0 ng/mL. This indicates a much higher chance of cancer.
This chart shows prostate cancer detection rates across different PSA levels:
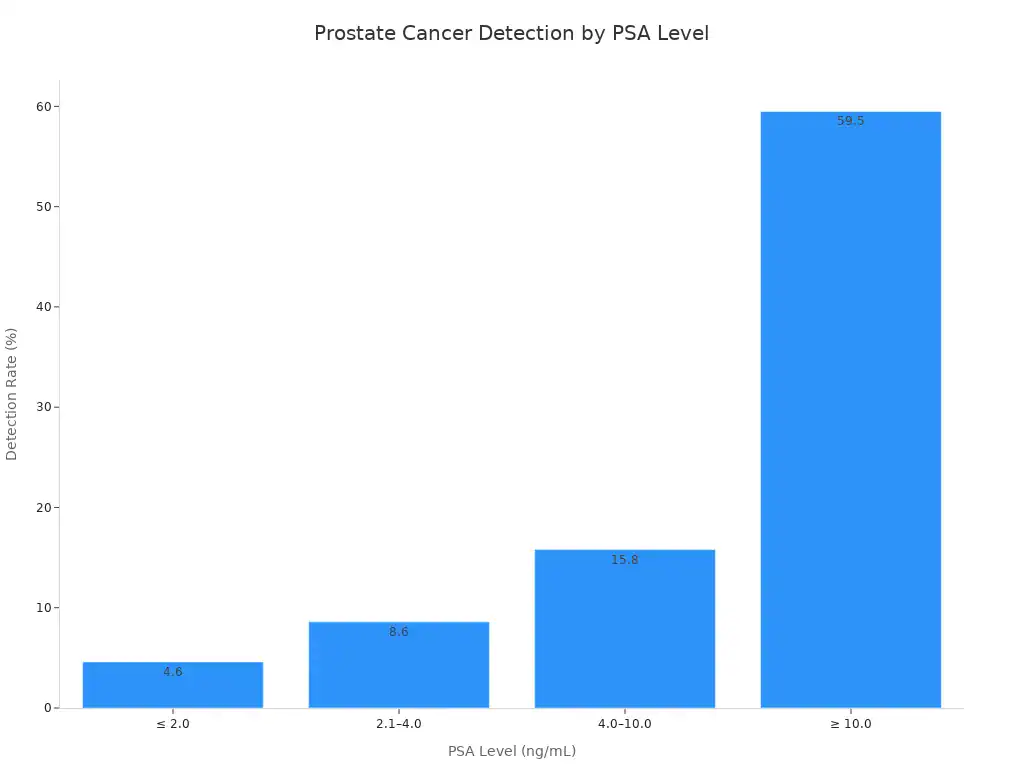
You can see that high PSA levels significantly increase the detection rate. For example, a PSA level between 4.0–10.0 ng/mL has a 15.8% detection rate. A PSA level of ≥ 10.0 ng/mL has a 59.5% detection rate. Your doctor may also look at PSA velocity (how fast your PSA changes) and PSA density (PSA divided by prostate volume) for a more complete picture.
Interpreting PSA Results
You receive your PSA test results. What do these numbers really mean for you? Understanding your prostate health goes beyond just looking at a single PSA number. Doctors consider several factors to get a complete picture.
Beyond the PSA Number
Your total PSA level is important. However, doctors also look at other PSA measurements. One key measurement is the percent free PSA (%fPSA). This value shows the ratio of free PSA to total PSA in your blood. Manufacturers typically provide this value directly. It usually falls between 5% and 75%.
The Prostate Cancer Prevention Trial Risk Calculator Version 2.0 uses percent free PSA as a key input. This helps assess your prostate cancer risk. A lower percentage of free PSA often means a higher risk of clinically significant prostate cancer.
Look at this table. It shows how %fPSA relates to cancer detection:
%fPSA Category | CSC Detection Rate | Number of Patients |
|---|---|---|
< 17.6% | 34% | 94 |
> 17.6% | 4% | 114 |
Note: This study involved patients with PI-RADS <3 and PSA ≤10 ng/ml. A %fPSA cutoff of 17.6% showed a sensitivity of 86.5% and specificity of 63.7% for detecting clinically significant prostate cancer.
This chart further illustrates the difference:
You can see that a %fPSA below 17.6% has a much higher cancer detection rate.
PSA Velocity and Density
Doctors also consider how your PSA levels change over time. This is called PSA velocity (PSAV). They also look at PSA density (PSAD).
PSA velocity measures how fast your PSA levels rise each year. Its role in predicting prostate cancer progression is not always clear.
Some studies show mixed results. For example, Whitson et al. found no significant role for PSAV in predicting progression for men on active surveillance. Ross et al. also found PSAV was not a strong predictor.
Other studies show a link. Ng et al. found PSAV connected to adverse histology. Kotb et al. observed PSAV correlated with tumor progression on later biopsies.
PSAV might predict tumor progression in specific groups. Iremashvili et al. found this in men undergoing their fourth biopsy.
Pre-diagnostic PSAV over 2 ng/mL/year or 3 ng/mL/year was linked to future biopsy progression risk. However, this link became less clear after adjusting for baseline PSA density.
This table shows various study findings on PSAV:
Study | Intervention Type | Endpoint | Main Results Related to PSAV |
|---|---|---|---|
Freedland et al. | Radical prostatectomy | Pathologic features or biochemical recurrence | Preoperative PSAV was not predictive of positive surgical margins, capsular penetration, seminal vesicle invasion, or biochemical recurrence. |
D’Amico et al. (44) | Radical prostatectomy | Death due to PC | Annual PSAV > 2.0 ng/ml associated with shorter time to death from PC. |
D’Amico et al. (45) | Radiotherapy | Death due to PC | Annual PSAV > 2.0 ng/ml associated with shorter time to death from PC. |
Sengupta et al. | Radical prostatectomy | Biochemical progression, clinical progression, death from PC | PSAV was a significant predictor for biochemical progression, clinical progression, and PC-specific death. |
Patel et al. | Radical prostatectomy | Relapse | Preoperative PSAV > 2 ng/ml/y predicted surgical stage, positive margins, pathologic grade, and relapse-free survival. |
Berger et al. | Radical prostatectomy | Biochemical progression | PSAV correlated significantly with tumor volume. |
Palma et al. | Not specified | Biochemical disease-free survival | PSAV > 2.0 ng/mL/year associated with reduced biochemical disease-free survival. |
Datan et al. | Radical prostatectomy | Positive bone scan | Preoperative PSAV predicted a positive bone scan (OR 0.93). |
Helfand et al. | Various prostate surgeries | Incidental PC | Patients with PC had significantly higher postoperative PSAV compared to those without PC. |
PSA density (PSAD) is another tool. You calculate PSAD by dividing your serum PSA level by the volume of your prostate gland. Doctors measure prostate volume using imaging like transrectal ultrasound (TRUS) or MRI. PSAD helps predict prostate cancer. It guides decisions between active surveillance and more aggressive treatments. Common threshold values for PSAD are 0.15 or 0.20 ng/mL².
Next Steps for Elevated PSA
You have elevated PSA levels. What happens next? Your doctor will recommend further tests to understand why your PSA is high.
Here are common follow-up steps:
Repeat your PSA blood test. This confirms if the levels remain high.
Get a general health assessment. This includes checking kidney, bone, and liver function. Doctors also check your blood cell count for issues like anemia.
Have a urine test. This rules out infection as a cause for your elevated PSA.
Undergo a prostate examination. This is not always essential for further testing referral.
Your doctor may refer you to a urologist. This often happens quickly through a fast-track system.
You might get an MRI scan of your prostate.
A prostate biopsy may be necessary. This is especially true if your MRI looks suspicious or unclear. It also happens if concerns remain despite a clear MRI.
A prostate biopsy helps diagnose prostate cancer. However, it carries potential risks and benefits.
Potential Outcome | Number of Men (out of 1,000 screened over 13 years) |
|---|---|
Deaths from prostate cancer avoided | 1.3 (or 1 per 769 men screened); up to 2 (or 1 per 570 men screened) |
Avoided metastatic cancer | 3 |
Died from prostate cancer despite screening/treatment | 5 |
Positive PSA test result (many false-positives) | 240 |
Biopsy with bothersome symptoms (pain, bleeding, infection) | Some men (2 hospitalized) |
Diagnosed with prostate cancer | 100 |
Treated for prostate cancer (surgery/radiation) | 80 |
Serious complication from treatment (e.g., sexual dysfunction) | 50 |
Urinary incontinence from treatment | 15 |
Died from other causes | 200 |
This chart shows outcomes for 1,000 men over 13 years:
Biopsies can lead to overdiagnosis and overtreatment. This means finding slow-growing cancers that would not cause problems. Unnecessary treatments can cause side effects. These include urinary, bowel, and sexual dysfunction. Examples are leaking urine, frequent urination, loose stools, rectal bleeding, and erectile dysfunction. False-positive PSA results also occur. These are elevated PSA levels without cancer. They cause anxiety and lead to unnecessary biopsies. Biopsy side effects include serious infections, pain, and bleeding. About 6-7% of men have a false-positive PSA. Only about 25% of men with elevated PSA undergoing biopsy have cancer.
Avoiding unnecessary prostate biopsies prevents complications. These include:
Hematuria (blood in urine)
Perineal or rectal discomfort
Urinary retention
Potentially fatal infectious complications, like sepsis.
A 2011 study showed an increase in fluoroquinolone-resistant Escherichia coli. It also showed a tripling of hospitalization rates for infectious complications to 3%. In that study, 44 men had adverse events. Eight men (1%) developed sepsis. Fifty-eight men (10%) experienced urinary retention.
Screening for Prostate Cancer
Prostate cancer screening involves regular PSA testing. Guidelines for prostate cancer screening vary by age and risk factors. You should discuss these with your doctor.
Here are guidelines from major bodies:
Guideline Body | General Population Screening | Increased Risk Population Screening |
|---|---|---|
AUA | Shared decision-making: Undergo PSA screening beginning at age 45–50 years | Undergo PSA screening beginning at age 40–45 years |
NCCN | Shared decision-making: Undergo PSA screening between age 45–75 years | Undergo PSA screening between age 40–75 years |
CUA | Shared decision-making: Undergo PSA screening ≥50 years | Undergo PSA screening ≥45 years |
USPSTF | Shared decision-making: Undergo PSA screening between 55–69 years; Against PSA screening >70 years | N/A |
You have an increased risk for prostate cancer if you:
Have a germline pathogenic or likely pathogenic variant in a prostate cancer-related gene.
Have a family history of prostate cancer in close relatives.
Are of Black/African American ancestry.
These factors mean you have a >25% lifetime risk for prostate cancer.
Here are general recommendations for screening:
Average Risk: Doctors may offer a baseline PSA test. You can begin prostate cancer screening between ages 45 to 50 years.
Increased Risk: Screening should start at age 40 to 45 years. This applies to individuals with factors like Black ancestry, germline mutations, or a strong family history of prostate cancer.
Regular Screening (Ages 50-69): You should have regular prostate cancer screening every 2 to 4 years.
Personalized Rescreening: Your rescreening interval can be personalized. It can also stop based on your preference, age, PSA levels, prostate cancer risk, life expectancy, and general health. This follows shared decision-making with your doctor.
For men 70 years and older, recommendations change. The Canadian Task Force on Preventive Health Care strongly recommends against screening for prostate cancer with the PSA test. This is for men 70 years and older. They base this on lower life expectancy and a lack of evidence for benefit. They also note evidence of harms in this age group. The U.S. Preventive Services Task Force (USPSTF) also recommends against PSA-based screening for prostate cancer in men 70 years and older. Doctors should not routinely screen men in this age group.
Proactive Prostate Health

Taking charge of your prostate health is important. You can make lifestyle choices and follow screening advice. This helps you maintain a healthy prostate.
Lifestyle for a Healthy Prostate
Your daily habits greatly impact your prostate. Eating a healthy diet can reduce your prostate cancer risk. Focus on nutrient-dense foods. Studies show a healthy dietary pattern lowers prostate cancer risk. A Mediterranean diet, rich in fruits, vegetables, nuts, legumes, and whole grains, protects against prostate cancer. This plant-based approach also reduces chronic disease risk. A “Prudent” diet, high in non-starchy vegetables and whole grains, also links to lower prostate cancer risk.
Physical activity also benefits your prostate. Regular exercise can lower your risk of prostate cancer progression and mortality. Try cardio exercises like jogging, walking, or swimming. Include lower body strength training with squats and lunges. Core strength training, like planks, also helps. Kegel exercises strengthen pelvic muscles. Yoga poses can improve prostate health. Even brisk walking for three hours a week can reduce cancer progression by 57%. Vigorous activity, like cycling or swimming, for more than three hours weekly links to lower prostate cancer-related mortality.
Regular Screening Guidelines
Following a regular screening schedule is key for early detection. If your PSA levels are less than 2.5 ng/mL, you may only need retesting every two years. For men aged 70 and older, the U.S. Preventive Services Task Force (USPSTF) recommends against PSA-based screening for prostate cancer.
For men with a family history of prostate cancer, current evidence does not strongly support specific screening recommendations. Screening based solely on family history might miss many cancers. For men of African descent, evidence for optimal screening intervals is weak. However, adapting screening intervals based on your current PSA levels can help. The American Cancer Society suggests biennial screening if your PSA is less than 2.5 ng/mL. They recommend annual screening if your PSA is more than 2.5 ng/mL.
Consulting Your Doctor
Talking to your doctor about your prostate health is crucial. Prepare information to share. Tell your doctor about any symptoms you have. Note how often they occur and their impact on your daily life. Share your personal and family medical history. List all current medications and supplements.
You should also prepare questions for your doctor. Ask about your risk of developing prostate cancer. Inquire about tests you might need and how often you should be screened. Ask about the benefits and harms of a PSA test and digital rectal exam (DRE). Understand what normal and abnormal results mean. If you have elevated PSA levels, ask about your specific PSA level and how fast it has risen. Discuss your prostate cancer Grade Group and what it means for your treatment approach.
This prostate health guide helps you understand your PSA levels. They are a key part of your overall prostate health. Always discuss your PSA results with a doctor. They consider your individual health history and risk factors. This reduces your risk of misinterpretation. Engage proactively with your prostate health. Get regular screenings. Talk openly with your doctors about your PSA. Remember, your PSA is just one piece of the puzzle. Effective management and treatment options are available for prostate issues. This comprehensive prostate health guide empowers you.




