You have probably experienced back pain at some point. Diagnosing its cause can be tricky. Studies show up to 20% of hip pain cases are initially misdiagnosed as lower back pain due to overlapping symptoms. How do you tell the difference between a herniated disc vs muscle strain? These conditions have key differences. A herniated disc often causes radiating pain and nerve involvement. A muscle strain typically results in localized pain. Understanding these distinctions helps you identify your specific issue.
Key Takeaways
A muscle strain causes pain in one spot. A herniated disc often causes pain that spreads to other body parts, like your leg.
Numbness, tingling, or weakness in your arms or legs usually means you have a herniated disc. These symptoms do not happen with a muscle strain.
Muscle strains often get better with rest in a few weeks. Herniated disc pain can last longer and may need more treatment.
See a doctor if your back pain is very bad, does not go away, or causes problems like weakness or loss of bladder control. These are serious signs.
Understanding Muscle Strain

Defining Muscle Strain
A muscle strain, often called a pulled muscle, happens when you stretch or tear your muscle fibers. This common injury occurs when you pull a muscle too hard or overuse it. This action weakens the fibers. A muscle strain involves the stretching or tearing of these fibers. These injuries typically occur when you stretch a muscle beyond its capacity. They also happen when you force a muscle to contract too strongly. The severity of a muscle strain can range from a few stretched fibers to a complete tear. This complete tear can stop the muscle from working.
Causes of Muscle Strain
Many activities can cause a muscle strain in your back or other areas. You might experience a muscle strain from explosive actions, like sprinting. Sudden increases in your exercise routine can also lead to this type of back pain. Muscles can become over-fatigued, for example, during intense training. Activities requiring explosive movements, such as pushing off in a sprint, often cause a muscle strain. Excessive loading of the muscle, especially when it contracts while elongating, also contributes. Starting a new sport or greatly increasing your exercise load can also cause a muscle strain.
Muscle Strain Pain Characteristics
Pain or tenderness is a main symptom of a strained muscle. This pain often gets worse with specific movements. Some people feel a continuous dull ache. You will also feel tenderness around the affected muscle, especially when you press on it. Muscle strains show a range of symptoms, including increasing pain and severe soreness. You might also feel throbbing and tenderness. The severity of your pain and other symptoms depends on the grade of the muscle strain.
Common Muscle Strain Symptoms
You might feel mild pain and some swelling with a mild muscle strain. This happens when muscle fibers stretch with small tears. A moderate muscle strain brings moderate pain and swelling. You will also notice tenderness, bruising, and limited movement.
This results from several torn muscle fibers. A severe muscle strain often causes a ‘pop’ sensation when the injury happens. You will have significant pain, bruising, tenderness, and swelling. Your movement will be very limited. You might even see a ‘dent’ or ‘gap’ where most or all muscle fibers tore. Other common symptoms include muscle weakness and difficulty walking. You might also have increased pain when you use the injured back muscle.
Muscle Strain Recovery
For most people with mild muscle strains, the healing period is about 2 to 4 weeks. Mild muscle strains usually heal within a few days to a week. These strains involve minor damage to muscle fibers. They cause mild pain and swelling. A Grade 1 muscle injury generally recovers within 1 to 3 weeks. Rest helps your back muscle recover from this type of pain.
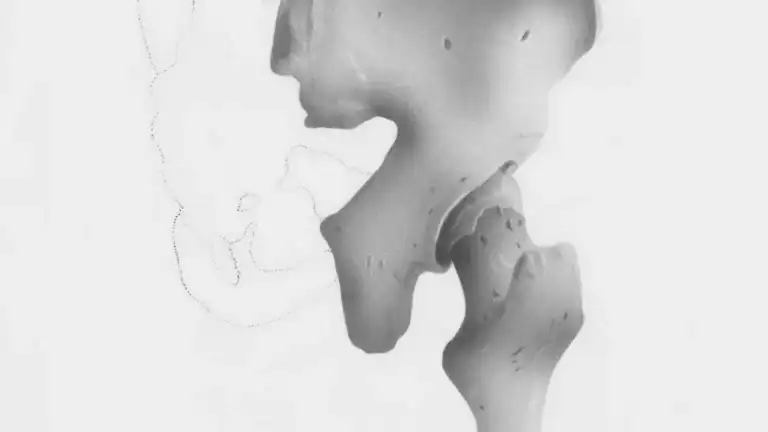
Understanding Herniated Disc

Defining a Herniated Disc
A herniated disc occurs when the intervertebral disc ruptures. Its jelly-like center spills into the spinal canal. This condition is also known as a slipped disc or a ruptured disc. You have discs between your vertebrae. These discs act as cushions. A herniated disc means one of these cushions has a problem.
Term | Description |
|---|---|
Herniated Disc | The intervertebral disc ruptures, releasing its jelly-like center into the spinal canal. |
Disc Bulge | A broad-based ballooning of the disc into the spinal canal, caused by weakening of the outer layer (annulus) without a full rupture. It is less severe than a true herniation. |
Causes of a Herniated Disc
Many things can cause a herniated disc. Heavy lifting puts excessive strain on your lower back. This can rupture a disc’s outer layer. Repetitive movements, especially those involving your back, can damage discs over time.
Sports injuries, like sudden trauma from falls, also lead to herniation. Your discs naturally weaken with age. They dry out, making them more prone to rupture from minor strain or twisting. You might also have a genetic predisposition for a herniated disc.
Herniated Disc Pain Characteristics
A herniated disc often causes specific types of pain. You might feel sharp or dull pain in your back near the affected disc. This pain can occur whether you are active or resting. You may experience burning, tingling, or numbing sensations. These symptoms often follow the nerve pathway.
For example, a neck herniation can cause symptoms in your arms and hands. A lower back pain herniation can cause symptoms in your legs, buttocks, and feet. You might also have muscle weakness. This makes activities like climbing stairs difficult.
Nerve Irritation from Herniated Disc
A herniated disc causes nerve irritation in several ways. The disc material can directly press on adjacent nerve roots. This is mechanical irritation. Your body also sees the herniated material as foreign.
It starts an immune response. Immune cells release inflammatory chemicals around the nerves. These chemicals cause nerve inflammation. This leads to pain, numbness, or weakness. Inflamed nerves can also trigger muscle spasms.
Factors Worsening Herniated Disc Pain
Certain activities worsen herniated disc pain. High-impact activities like running or heavy weightlifting jolt your spine. This increases stress on the herniated disc and intensifies your pain.
Poor posture, like slouching, shifts spinal alignment. This puts more pressure on the herniated disc. Prolonged sitting, especially in non-ergonomic chairs, also puts excessive pressure on your lower spine. Improper lifting techniques, such as bending at the waist, strain your back. Being overweight increases the load on your spine.
Differentiating Herniated Disc vs Muscle Strain
Understanding the differences between a herniated disc vs muscle strain is crucial for proper treatment.
You need to pay close attention to your specific symptoms. While both conditions cause back pain, their origins and how they affect your body are quite distinct. Knowing these differences helps you understand what is happening in your back.
Pain Location and Type Differences
The location and type of your pain offer major clues. A muscle strain typically causes localized pain. This means you feel the pain directly in the injured muscle. It usually does not spread to other areas. A herniated disc, however, often causes pain that travels. This radiating pain is a key indicator.
Consider these differences in pain location:
Condition | Pain Location |
|---|---|
Herniated Disc | Pain often radiates from the lower back down the leg, sometimes into the foot. It can also occur in the neck, shoulders, and arms. |
Muscle Strain | Pain is typically localized to the affected muscle in the back. It usually doesn’t radiate to other areas. |
You might feel a deep ache or a sharp tugging sensation with a muscle strain. This pain usually stays in one spot in your back. With a herniated disc, you often experience sharp, shooting, or electric-like pain. This pain follows a nerve path. For example, you might feel it from your lower back down your leg.
Nerve Symptoms as a Differentiator
Nerve-related symptoms are the most significant differentiator between a herniated disc and a muscle strain. A muscle strain typically does not involve your nerves. Therefore, you will not experience nerve symptoms. A herniated disc, however, often presses on or irritates nearby nerves. This causes a range of specific symptoms.
You might experience these nerve-related symptoms with a herniated disc:
Radiating Pain: This pain can travel down your arm if you have a neck herniation. It can also go from your buttocks to your thigh, calf, or foot if you have a lower back pain herniation. This pain follows the nerve path. It can be sharp or dull. It might be constant or come and go. Actions like sitting or standing often make this pain worse.
Electric or Burning Pain: You might feel this pain in your back. It can also spread around your chest or abdomen. Sometimes, it radiates into your legs.
Numbness and Tingling: You often feel these sensations in the limbs affected by the herniation.
Muscle Weakness: You might notice reduced strength in your leg muscles. This can make walking difficult.
Sciatica: This is a specific type of radiating pain. It travels along the sciatic nerve from your lower back down your leg.
This table further highlights the differences in symptoms:
Symptom Type | Herniated Disc | Muscle Strain |
|---|---|---|
Pain Character | Radiating (e.g., sciatica), sharp, shooting, electric-like | Localized, deep ache, sharp tugging |
Neurological Symptoms | Numbness, tingling, weakness, altered reflexes | Typically absent |
Pain Location | Along nerve path (arm, leg) | Confined to injured muscle/tendon |
Aggravating Factors | Nerve compression, certain positions | Movement, palpation |
Associated Signs | None typically mentioned | Mild swelling, bruising, muscle spasms |
Onset and Duration of Pain
The way your pain starts and how long it lasts can also help you tell the difference. A muscle strain often has a sudden onset. You might feel a “pop” or immediate pain during an activity. This pain usually improves with rest and time. Most muscle strain injuries heal within a few weeks.
A herniated disc can also start suddenly, especially after heavy lifting. However, the pain from a herniated disc can sometimes develop more gradually. It might worsen over days or weeks. This type of back pain can also be more persistent. It may not improve easily with simple rest.
Associated Symptoms Beyond Pain
Beyond the main pain, other symptoms can help you distinguish between these two conditions. With a muscle strain, you might notice mild swelling or bruising in the affected back area. You could also experience muscle spasms. These spasms are the muscle tightening involuntarily. For a herniated disc, you might experience more severe symptoms. These include significant muscle weakness in your limbs. You might have difficulty lifting your foot or walking on your toes. Sometimes, you might notice altered reflexes in your legs or arms. These additional symptoms point more strongly towards a herniated disc affecting your nerves.
When to Seek Medical Advice for Back Pain
You need to know when your back pain requires professional attention. Sometimes, back pain is a minor issue. Other times, it signals a serious condition. Recognizing specific symptoms helps you decide when to see a doctor.
Red Flag Symptoms for Back Pain
Certain symptoms are critical warning signs. You should never ignore these “red flags.” They indicate a potentially serious underlying condition.
Loss of Bowel or Bladder Control: This is a critical warning sign. It suggests cauda equina syndrome. You need immediate emergency medical attention to prevent permanent paralysis.
Severe Back Pain Accompanied By Fever: This may indicate a spinal infection. Infections can progress rapidly. They can cause permanent neurological damage if you do not treat them.
Weakness in One or Both Legs: Progressive weakness, especially with numbness or tingling, suggests nerve compression. This may need urgent intervention, particularly if it develops rapidly.
Back Pain After Trauma: Any back pain following significant trauma, like a fall or accident, requires immediate evaluation. You could have spinal fractures or dislocations.
Numbness or Tingling in Both Legs: If this spreads down both legs simultaneously, especially with weakness, it indicates possible compression of multiple nerve roots or the spinal cord.
Changes in Reflexes, Coordination, or Balance: Difficulty walking, frequent falls, or problems with fine motor skills can signal spinal cord compression or other serious neurological conditions.
Severe Pain That Worsens When Lying Down: Pain that intensifies with rest or at night, rather than improving, may indicate serious underlying conditions. These include tumors, infections, or inflammatory issues.
Saddle Anesthesia: You experience numbness in the genital, buttocks, or inner thigh areas. This often accompanies cauda equina syndrome. It indicates compression of nerve roots controlling bowel, bladder, and sexual function.
Age <18 or >50: Age can be a risk factor for more serious conditions.
Pain Not Resolved by Analgesia: Your pain persists despite taking pain relief medication.
History of Trauma or Recent Spinal Interventions: You have back pain after an injury or spinal procedure.
Symptoms or History of Malignancy: You have signs like night sweats or weight loss, or a history of cancer.
History of Immunodeficiency, Recent Infection, or Fever: These conditions increase your risk of spinal infections.
When to See a Doctor for Back Pain
You should seek medical advice for back pain if you experience any of these symptoms:
Unexpected Weight Loss: You lose weight without trying.
Night Pain or Night Sweats: Your pain worsens at night, or you experience night sweats.
Fevers: You have a fever along with your back pain.
Loss of Bowel or Bladder Control: This is a serious sign.
Weakness in Your Arms or Legs: You notice new or worsening weakness.
Severe, Unrelenting Pain: Your pain is intense and does not go away.
Sharp Pain Rather Than a Dull Ache: This could indicate a torn muscle/ligament or an internal organ issue.
Radiating Pain: Your pain moves or shoots to your glutes or legs. This could signify nerve compression or damage, often associated with a herniated disc.
Difficulty Standing or Walking: You find it hard to move around.
Pain That Extends from the Lower Back Around to the Abdomen: This can indicate various issues.
Sudden Numbness in the Pelvic Region or in One or Both Legs: This is a serious neurological symptom.
Back pain that persists for more than two weeks: Your pain does not improve with self-care.
Back pain that prevents daily activities: You cannot do your normal routine.
Shooting pain down your arms or legs: This indicates nerve irritation or damage.
Nighttime pain that worsens: This suggests a potentially more serious underlying issue.
Fever over 101 degrees Fahrenheit accompanying persistent back pain: This may signal an infection.
Problems with balance or controlling bowels or bladder: These are signs of serious problems.
Diagnostic Methods for Back Pain
Doctors use various methods to diagnose the cause of your back pain. The diagnosis process helps determine if you have a muscle strain or a herniated disc.
For a muscle strain, the diagnosis often begins with:
Clinical History and Physical Examination: Your doctor asks about your injury and symptoms. They then inspect and palpate the affected muscles. They also perform function tests.
Ultrasound (US): This is often an initial method. It is affordable and accessible. It allows for dynamic evaluation of muscle contraction and rupture.
Magnetic Resonance Imaging (MRI): This provides detailed evaluation of muscle morphology. It helps classify muscle injuries and assess tissue healing.
X-ray: Doctors use X-rays to check for bone abnormalities. They can rule out fractures or other bone-related issues.
For a herniated disc, doctors often use these diagnostic tools:
Magnetic Resonance Imaging (MRI): This is the gold standard for diagnosing a herniated disc. It provides the most accurate assessment of the herniation’s location. It also shows affected neural tissue. Doctors prefer it for surgical planning.
Computerized Tomography (CT): This noninvasive X-ray procedure creates 3D images of your spine. It can show evidence of a ruptured disc.
Myelogram: This specialized X-ray involves injecting dye into your spinal fluid. It helps identify a ruptured disc. Doctors often follow it with a CT scan.
Electromyogram and Nerve Conduction Studies (EMG/NCS): These tests measure electrical activity in your nerves and muscles. They detect nerve damage or compression.
X-ray: While X-rays only show bones, they help check for bone-related issues like vertebral fractures.
General Treatment for Muscle Strain
You can often treat a muscle strain effectively at home. Initial treatment focuses on reducing pain and swelling.
R.I.C.E. Method:
Rest: Avoid activities that cause or worsen your pain.
Ice: Apply cold compresses or ice packs for 10-15 minutes at a time. This reduces swelling and pain.
Compression: Wrap the injured area with an athletic bandage. This helps reduce swelling.
Elevation: Elevate the affected area above heart level. This also reduces swelling. You should apply this method several times daily for the first few days. It is often sufficient for mild to moderate strains.
Medication: You can use anti-inflammatory medicines like ibuprofen, naproxen, or acetaminophen. These reduce pain and swelling.
Physical Therapy: Once your pain and swelling subside, physical therapy helps. It restores flexibility and strength.
You now understand the key distinctions between a herniated disc vs muscle strain. While both cause back pain, their underlying mechanisms and symptoms differ significantly. A muscle strain typically causes localized back discomfort or sharp back sensations.
A herniated disc often presents with radiating pain, numbness, or weakness. This type of pain can be severe. These specific symptoms are crucial indicators of a more serious back issue. Do not ignore persistent back discomfort or any new back sensations. Self-diagnosis of your back problems can be misleading. Professional medical evaluation is crucial for an accurate diagnosis and effective treatment plan for your back. This ensures proper recovery and prevents long-term complications from any back issue, alleviating your pain and discomfort.