
Many people experience unexplained pain or numbness. These symptoms often point to issues along the spine. A dermatome is a specific skin area. A single spinal nerve supplies sensation to this dermatome. Each spinal nerve connects to a distinct dermatome. These dermatomes form a vital spinal nerve chart.
It acts as a “dermatome pain map” for diagnosing nerve issues. This map helps pinpoint the source of pain. Understanding these dermatomes is crucial. It helps make sense of various body symptoms. This guide explains what dermatomes are, where they are, and why they are vital for understanding body pain and conditions affecting the spine and spinal nerves.
Key Takeaways
A dermatome is a skin area. A single spinal nerve supplies sensation to this area. This helps doctors find nerve problems.
Dermatome charts map the body’s sensory input. They show which spinal nerve connects to each skin area. This helps diagnose nerve damage.
Doctors use dermatomes to find nerve issues. They check for numbness or pain. This helps them treat conditions like pinched nerves.
Many conditions affect dermatomes. These include radiculopathy, shingles, and spinal cord injuries. Each condition shows symptoms in specific dermatome areas.
Dermatome pain patterns can vary. Doctors combine dermatome tests with other exams. This helps them make an accurate diagnosis.
What is a Dermatome: Your Spinal Nerve Chart
Defining Dermatomes
A dermatome is a specific area of skin. This area receives its sensory innervation from a single spinal nerve root or spinal segment. Medical professionals define a dermatome as an area of skin mainly supplied by afferent nerve fibers. These fibers come from the dorsal root of a given spinal nerve.
It is also an area of skin supplied by sensory neurons. These neurons arise from a spinal nerve ganglion. The term “dermatome” comes from Greek words: “derma” (skin) and “tome” (segment). This defines a segment of skin. Its sensory input comes from a single spinal segment, spinal nerve, or nerve root.
The human body has 31 pairs of spinal nerves. However, only 30 such areas are typically associated with these nerves. The C1 spinal nerve usually lacks a sensory root. Each dermatome links to a single spinal nerve.
These areas create a detailed spinal nerve chart. This chart acts as a map. It represents areas of skin with specific nerve connections. This dermatome chart helps understand where sensory information travels to the spine. Understanding these segments is key to mapping the body’s sensory input to the spine.
Spinal Nerves and Sensory Function
Spinal nerves play a crucial role in sensory perception. They conduct sensory information from various parts of the body to the central nervous system. The posterior root of each spinal nerve is primarily sensory. It contains axons from sensory end organs. These nerves distribute to sensory receptors for touch, pain, and temperature. They also innervate muscles and joints. This allows them to sense tone and position.
Each of the many dermatomes on the body surface connects to a specific spinal nerve. These spinal nerves carry signals from the skin to the spine. The health of the spine directly impacts these nerves and the dermatomes they serve. For example, sacral nerves are responsible for sensory perception in the pelvic organs. They conduct sensory information from the descending colon, rectum, urinary bladder, and genital organs to the central nervous system.
The intricate network of spinal nerves ensures that the brain receives constant updates about the body’s external and internal environment. This system of dermatomes provides a clear pathway for sensory signals up the spine. Understanding these dermatomes helps in diagnosing issues related to the spine.
Mapping Dermatomes: The Body’s Sensory Chart
Clinicians use a visual dermatome chart to understand sensory pathways. This section outlines areas of skin innervated by sensory fibers from specific spinal nerve roots. Each dermatome represents a distinct region. These regions help map sensory input to the spine.
Cervical Dermatomes: Neck and Arms
Cervical dermatomes cover the neck, shoulders, and arms. These dermatomes are supplied by cervical spinal nerves. The C2 dermatome covers the upper part of the head. The C3 dermatome covers the side of the face and back of the head. C4 covers parts of the neck, shoulders, and upper arms.
The C5 dermatome covers the outer part of the upper arm down to the elbow. C6 covers the thumb side of the hand and forearm. The C7 dermatome goes down the back of the arm and into the middle finger. C8 covers the pinky side of the hand and forearm. (The C1 spinal nerve usually has no sensory dermatome.)
Dysfunction in these cervical dermatomes can cause specific sensory symptoms. Patients often experience impaired sensation. Doctors assess this with a pinprick test. This test helps distinguish areas of diminished sensory function. For example, cervical radiculopathy often causes impaired sensation in the distal forearm and hand.
Radiculopathy Level | Common Sensory Loss Location |
|---|---|
C5 | Lateral upper arm |
C6 | Thumb and index finger |
C7 | Posterior forearm and third finger |
C8 | Fifth finger |
Thoracic Dermatomes: Trunk and Chest
Thoracic dermatomes cover the trunk and chest. These dermatomes are supplied by thoracic spinal nerves. They form horizontal bands around the body. These bands wrap around to the front. Issues with these spinal nerves can cause distinct symptoms. Patients may feel burning or shooting pain.
This pain can occur in the back, scapula, chest, or abdominal wall. A common complaint is “band-like” chest wall pain. This pain follows a dermatomal pattern. Coughing or straining can worsen the pain. Sensory deficits, like loss of sensation, also occur. Numbness, tingling, and dysesthesias are common. Pruritus, or itching, can also happen. These symptoms show problems with the spinal nerves in the spine.
Lumbar Dermatomes: Lower Body
Lumbar dermatomes cover the lower body. These dermatomes are supplied by lumbar spinal nerves. They include the hips, groin, and legs. Each dermatome links to a single spinal nerve. This spinal nerve transmits sensations like pain from a specific skin area to the central nervous system.
The body has 30 dermatomes, starting from spinal nerve C2. The C1 spinal nerve typically lacks a sensory root. Dermatomes have a segmented distribution. They show horizontal patterns on the torso and vertical patterns on the limbs. The exact pattern can vary between individuals.
Nerve | Roots | Sensory Functions |
|---|---|---|
Iliohypogastric nerve | L1 | Skin over the iliac crest, upper gluteal region, and hypogastric region. |
Ilioinguinal nerve | L1 | Skin over the upper medial thigh, root of the penis and anterior scrotum in males, and mons pubis and labia majora in females. |
Genitofemoral nerve | L1, L2 | Genital branch: Skin of the anterior scrotum in males and mons pubis and labia majora in females. Femoral branch: Skin of the upper anterior thigh. |
Lateral cutaneous nerve of thigh | L2, L3 | Skin over the anterior and lateral aspects of the thigh. |
Femoral nerve | L2, L3, L4 | Skin over the anterior thigh and medial side of the leg (via the saphenous nerve). |
Obturator nerve | L2, L3, L4 | Skin over the medial side of the thigh. |
Lumbar dermatome dysfunction often causes specific sensory symptoms. These include spontaneous burning pain and prickling sensations. Patients may experience pain from light touch (allodynia). Spontaneous pain attacks are also common. Pain from thermal stimuli and slight pressure can occur. Numbness is a frequent symptom. Severe pain attacks can feel like shooting pain. This pain travels along the lower limb. Slight movements of the lumbar spine can trigger it. Tingling or numbness in the affected area is also common.
Sacral and Coccygeal Dermatomes: Pelvis and Perineum
Sacral and coccygeal dermatomes cover the pelvis and perineum. These dermatomes are supplied by sacral and coccygeal spinal nerves. The Pudendal nerve (S2, S3, S4) innervates the skin of the perineum and external genitalia.
The Posterior cutaneous nerve of thigh (S1, S2, S3) covers the skin of the buttock, posterior thigh, and popliteal fossa. The Perforating cutaneous nerve (S2, S3) supplies skin over the medial and inferior part of the buttock. These dermatomes are crucial for sensation in these sensitive areas. Problems with these spinal nerves can lead to sensory loss or pain in the pelvic region. A comprehensive dermatome chart helps identify the specific spinal nerve affected.
Dermatome Pain: Diagnostic Significance

Pinpointing Nerve Issues
Dermatomes offer a crucial tool for doctors. They help pinpoint the location of nerve damage along the spine. Doctors test specific dermatomes for changes in sensation. These changes include numbness, tingling, or increased sensitivity. This process helps them diagnose conditions like pinched nerves, herniated discs, and spinal cord injuries.
Clinicians use dermatome maps to diagnose and treat nerve issues with high accuracy. These maps help pinpoint the location of spinal cord injuries or compressions. They also assist in assessing and diagnosing conditions such as injuries, cysts, tumors, and infections.
A dermatome chart guides doctors in understanding nerve distribution throughout the body. When a spinal nerve is irritated, injured, or compressed, it affects the body parts it connects to.
This understanding allows healthcare providers to identify the root of the problem. Consequently, they can diagnose health problems. The dermatome map assists doctors in speeding up diagnosis. It ensures patients undergo the correct tests, such as CT scans, MRIs, and nerve conduction studies, at the appropriate time. Knowledge of dermatome locations also helps surgeons avoid nerve damage during spinal surgery. This minimizes post-surgical complications.
Identifying Pain Sources
Understanding which dermatomes correspond to specific body regions helps doctors identify the source of pain. For example, a burning sensation along the side of the chest might indicate a problem with a specific thoracic spinal nerve root.
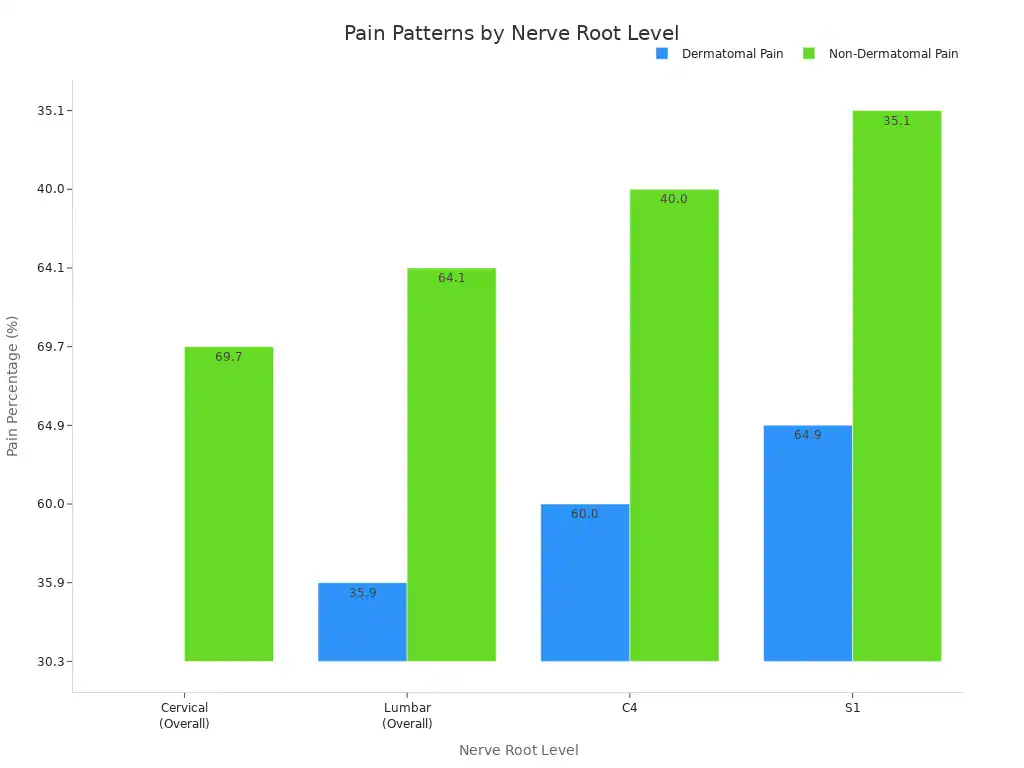
However, the diagnostic accuracy of dermatome pain patterns for identifying nerve root compression is not always high. Studies show that only about 62.6% of patients with cervical radiculopathy present with a standard dermatomal pattern.
Another study reported that only 54% of patients showed radiating pain and numbness following the standard dermatomal pattern. This variability means that in specific radiculopathy groups, the percentage of patients showing a typical dermatomal pattern ranges from 60.0% to 66.6%. Many patients experience atypical or poorly localized pain.
There is high variability in human dermatomes. Many neurological symptoms used to determine cervical pathological levels do not possess high diagnostic accuracy in real-world scenarios.
Experienced cervical spine surgeons acknowledge that only about half of cervical radiculopathy patients exhibit a ‘typical’ pattern of clinical symptoms. This means doctors must carefully correlate imaging findings with neurological examinations.
Patients with severe nerve root compression on MRI may not always present with corresponding symptoms. While dermatome testing effectively detects sensory changes from nerve root damage, its accuracy can be limited. It may not fully assess motor dysfunction. Therefore, combining dermatomal testing with other clinical assessments provides a more comprehensive diagnosis.
Nerve root pain generally does not follow a specific dermatomal pattern. This makes it an unreliable diagnostic factor. The primary exception is S1 radicular pain, which often follows the S1 dermatome.
For other nerve root levels, the pain pattern is largely non-dermatomal. The quality of pain (e.g., aching, sharp, burning) is also generally not a sensitive or specific indicator for diagnosing nerve root pain. Scapular pain is common in cervical radicular pain, especially with herniated discs. However, its diagnostic utility for nerve root pain itself is low.
Nerve Root Level | Dermatomal Pain (%) | Non-Dermatomal Pain (%) | Sensitivity (Dermatomal Pattern) | Specificity (Dermatomal Pattern) |
|---|---|---|---|---|
Cervical (Overall) | 30.3 | 69.7 | Low | Low |
Lumbar (Overall) | 35.9 | 64.1 | Low | Low |
C4 | 60.0 | 40.0 | 0.60 | 0.72 |
S1 | 64.9 | 35.1 | 0.65 | 0.80 |
Clinical Assessment Tools
Dermatome assessment forms a key part of neurological examinations. This is especially true when doctors suspect radiculopathy. It involves using a brush, often found on reflex hammers.
Doctors stroke dermatome regions on both affected and unaffected limbs. They then ask patients to report any site-by-site differences in sensation. While its clinical value is considered somewhat weak, it remains the most effective physical assessment tool available.
It helps identify pathological disc levels, especially in the lower extremity. Nerve root compromise frequently occurs at L4/L5 and L5/S1 levels in the spine. These sensory dermatomes provide valuable clues.
Doctors also use other methods to test dermatomes. They might use a pinprick test to check for pain sensation.
A light touch test with cotton wool checks for touch sensation. Comparing sensations on both sides of the body helps identify differences. These differences can point to nerve issues in the spine. Combining these simple tests with a patient’s reported symptoms and medical history helps doctors form a complete picture. This comprehensive approach leads to a more accurate diagnosis and effective treatment plan.
Conditions Affecting Dermatomes
Radiculopathy
Radiculopathy occurs when a nerve root in the spine becomes pinched or irritated. This condition often causes pain, numbness, or weakness in the body area that specific nerve supplies.
Cervical radiculopathy, affecting the neck, impacts about 100 per 100,000 males and 60 per 100,000 females annually. Lumbar radiculopathy, in the lower back, affects 3-5% of the general population.
These conditions directly relate to dermatomes because the affected nerve root corresponds to a specific dermatomal region. The symptoms a person experiences often follow the pattern of the dermatome connected to the irritated nerve. This helps doctors locate the problem along the spine.
Shingles
Shingles is a viral infection that causes a painful rash. The varicella-zoster virus (VZV), which also causes chickenpox, causes shingles.
After a person has chickenpox, VZV stays dormant in nerve cells in the spine. When the virus reactivates, it travels down sensory nerves to the skin. This causes the characteristic rash and pain along a specific dermatome. About 1 in 5 people who had chickenpox will develop shingles. The initial symptom is often localized pain, even before any rash appears. This pain follows the path of one or more sensory nerves.
Neuropathies
Neuropathies involve damage to nerves outside the brain and spinal cord. These conditions can affect one or many dermatomes.
Peripheral nerves are arranged along dermatomes. Damage to these nerves can impact sensory, motor, and autonomic nerve fibers. Doctors classify neuropathies as sensory, autonomic, or motor. Common causes include diabetes, traumatic injuries, infections, and exposure to toxins. Sometimes, the cause remains unknown. This is called idiopathic neuropathy. Neuropathies can cause various symptoms like numbness, tingling, or burning pain in the affected dermatomal areas.
Spinal Cord Injury
A spinal cord injury damages the spinal cord. This damage disrupts the transmission of nerve messages. It leads to changes in sensation and motor function below the injury level. Doctors use dermatome assessment to understand the injury’s extent.
The American Spinal Injury Association (ASIA) classification system uses sensory and motor assessments at 28 key points on each side of the body. These points correspond to dermatomes from C2 through S4-5. This helps classify injuries as complete or incomplete.
For example, abnormal patterns of tactile sensitivity can appear in dermatomes above the injury level. This shows how spinal cord injury impacts dermatomal sensation.




